CRISPR-Cas Genome Editing: Engineering Therapeutic Cells for Clinical Applications
This article provides a comprehensive overview of CRISPR-Cas genome editing technologies in therapeutic cell design for researchers, scientists, and drug development professionals.
CRISPR-Cas Genome Editing: Engineering Therapeutic Cells for Clinical Applications
Abstract
This article provides a comprehensive overview of CRISPR-Cas genome editing technologies in therapeutic cell design for researchers, scientists, and drug development professionals. It explores the foundational principles and evolution of CRISPR systems, examines current methodological approaches and clinical applications including ex vivo and in vivo strategies, addresses key challenges in optimization and safety such as delivery and off-target effects, and discusses validation frameworks and comparative efficacy with traditional gene editing platforms. The content synthesizes the most recent clinical trial data and technological advancements up to 2025, offering a strategic roadmap for translating CRISPR technologies into safe and effective cell therapies.
From Bacterial Immunity to Therapeutic Revolution: The Foundations of CRISPR-Cas Editing
The Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) system has revolutionized biological research and therapeutic development, transitioning from an obscure bacterial immune element to a Nobel Prize-winning technology within three decades. This evolution represents one of the most significant advancements in modern biotechnology, enabling precise manipulation of genetic material with unprecedented ease and accuracy. For researchers and drug development professionals, understanding this historical trajectory provides critical insights into both the current capabilities and future potential of genome-editing technologies in therapeutic cell design. The journey from fundamental discovery to therapeutic application exemplifies how basic biological research can transform into powerful clinical tools, ultimately leading to the development of transformative genetic medicines for previously untreatable conditions. This application note details the key discoveries, methodological breakthroughs, and experimental protocols that have defined the CRISPR revolution, with particular emphasis on its application in therapeutic cell engineering.
Historical Timeline of Key Discoveries
The development of CRISPR technology spans several decades of incremental discoveries, culminating in its recognition as a powerful genome-editing tool. The table below summarizes the pivotal milestones in this journey.
Table 1: Historical Timeline of Key CRISPR-Cas Discoveries
| Year | Discovery/Event | Key Researchers/Entities | Significance |
|---|---|---|---|
| 1987 | Identification of unusual repetitive DNA sequences in E. coli | Ishino et al. | Initial observation of what would later be recognized as CRISPR loci [1] |
| 2002 | Term "CRISPR" coined; proposed function in microbial immunity | Jansen, Mojica, others | Conceptual framework for understanding CRISPR biological function [1] |
| 2005 | CRISPR spacers derived from viral and plasmid DNA | Mojica, Pourcel, others | Experimental evidence supporting adaptive immunity hypothesis [1] |
| 2007 | First experimental demonstration of CRISPR immune function | Barrangou et al. | Confirmed CRISPR provides acquired resistance against viruses in bacteria [1] |
| 2011 | Discovery of tracrRNA and its essential role in Cas9 system | Charpentier et al. | Identified key RNA component for Cas9 complex assembly [2] |
| 2012 | CRISPR-Cas9 reprogrammed for genome editing in vitro | Doudna, Charpentier et al. | Developed simplified two-component system using single guide RNA (sgRNA) [2] [3] |
| 2013 | First application in eukaryotic cells | Zhang, Church | Demonstrated CRISPR worked in human and mouse cells [1] |
| 2020 | Nobel Prize in Chemistry awarded | Charpentier and Doudna | Recognition of revolutionary impact on life sciences [2] [3] |
| 2023 | First FDA-approved CRISPR therapy (Casgevy) | CRISPR Therapeutics/Vertex | Landmark regulatory approval for sickle cell disease and beta thalassemia [3] |
Early Discoveries: The CRISPR Locus
The initial discovery of CRISPR sequences occurred in 1987 when Japanese researchers observed unusual repetitive DNA sequences in the E. coli genome, though their function remained mysterious. Francisco Mojica, a microbiologist at the University of Alicante in Spain, subsequently identified similar sequences in archaea and coined the term "CRISPR" in 2002 [1]. His crucial insight came in 2005 when he recognized that the spacer sequences between repeats matched viral and plasmid DNA, leading him to hypothesize that CRISPR constituted an adaptive immune system in prokaryotes [1]. This foundational work established the conceptual framework for all subsequent CRISPR research, demonstrating how basic microbial genomics can reveal fundamental biological mechanisms with far-reaching applications.
Key Contributors Beyond Charpentier and Doudna
While Emmanuelle Charpentier and Jennifer Doudna received the Nobel Prize for their seminal work in developing the CRISPR-Cas9 tool, several other scientists made indispensable contributions to the field. Feng Zhang of the Broad Institute was the first to demonstrate CRISPR application in eukaryotic cells, a critical step for therapeutic development [1]. Virginijus Šikšnys independently discovered the programmable nature of Cas9, publishing work parallel to Charpentier and Doudna [1]. Additional key contributors include Luciano Marraffini, who established that CRISPR targets DNA rather than RNA, and Rodolphe Barrangou, who provided the first experimental evidence of CRISPR's immune function in bacteria [1]. This collaborative, international effort highlights how scientific breakthroughs often emerge from multiple research groups working concurrently on related problems.
The Molecular Mechanism of CRISPR-Cas9
Bacterial Immunity to Genetic Engineering
The CRISPR-Cas system functions as an adaptive immune system in bacteria, providing resistance against foreign genetic elements such as plasmids and phages. In its natural context, the system incorporates short sequences from invading viruses into the CRISPR lattice as "spacers" between repeats, creating a genetic memory of past infections [4]. When the same virus attacks again, the bacterium transcribes these spacers into short CRISPR RNAs (crRNAs) that guide Cas proteins to recognize and cleave matching viral DNA sequences, thus neutralizing the threat [4].
The revolutionary insight from Charpentier and Doudna was recognizing that this system could be simplified and repurposed for precise genome engineering. Their key innovation was combining the tracrRNA (trans-activating CRISPR RNA) discovered by Charpentier with the crRNA into a single guide RNA (sgRNA) [2]. This created a two-component system where the sgRNA directs the Cas9 nuclease to specific DNA sequences, and Cas9 introduces double-strand breaks at the target site [2]. The DNA repair mechanisms that cells then employ—either non-homologous end joining (NHEJ) or homology-directed repair (HDR)—enable researchers to either disrupt gene function or insert new genetic material [4].
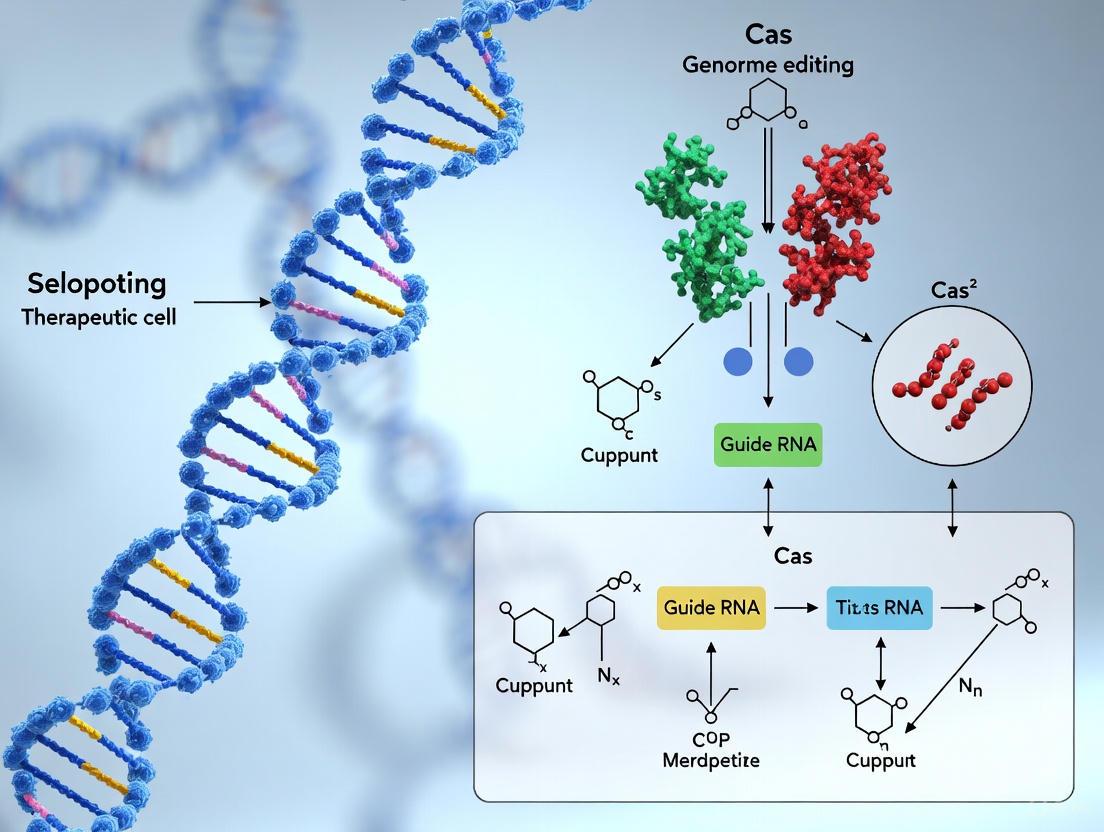
Diagram 1: CRISPR-Cas9 Molecular Mechanism. This workflow illustrates the sequential steps from complex formation through DNA repair pathways that enable genome editing.
Experimental Protocol: Basic CRISPR-Cas9 Genome Editing
Protocol Title: CRISPR-Cas9 Mediated Gene Knockout in Mammalian Cells
Principle: This protocol enables targeted gene disruption by introducing double-strand breaks in DNA via the CRISPR-Cas9 system, followed by repair through the error-prone non-homologous end joining (NHEJ) pathway, resulting in insertion/deletion mutations (indels) that disrupt gene function.
Materials:
- Mammalian cell line of interest
- Plasmid vectors expressing Cas9 and sgRNA or Cas9-sgRNA ribonucleoprotein complexes
- Transfection reagents (e.g., lipofectamine, electroporation system)
- Cell culture media and supplements
- PCR reagents and gel electrophoresis equipment
- Surveyor or T7 endonuclease I for mutation detection
- DNA sequencing primers
Procedure:
sgRNA Design and Synthesis
- Identify 20-nucleotide target sequence adjacent to 5'-NGG-3' PAM sequence
- Design sgRNA with high on-target and low off-target activity using computational tools (e.g., CRISPRscan, ChopChop)
- Synthesize sgRNA as DNA oligonucleotides for cloning into expression vectors or as in vitro transcribed RNA
Delivery of CRISPR Components
- For plasmid-based delivery:
- Clone sgRNA into Cas9 expression vector (e.g., pX330)
- Transfect cells using appropriate method (lipofection, electroporation)
- Include fluorescent marker or antibiotic resistance for selection
- For ribonucleoprotein (RNP) delivery:
- Complex purified Cas9 protein with in vitro transcribed sgRNA (3:1 molar ratio)
- Deliver via electroporation (recommended for primary cells)
- For plasmid-based delivery:
Analysis of Editing Efficiency
- Harvest cells 72-96 hours post-transfection
- Extract genomic DNA using standard protocols
- Amplify target region by PCR (amplicon size: 400-800 bp)
- Detect indels using:
- Surveyor/T7E1 Assay: Digest heteroduplex DNA with mismatch-sensitive nucleases
- Tracking of Indels by Decomposition (TIDE): Sequence PCR products and analyze decomposition profile
- Next-generation sequencing: Most comprehensive method for quantifying editing efficiency
Validation of Functional Knockout
- Isolate single-cell clones by limiting dilution or fluorescence-activated cell sorting
- Expand clones for 2-3 weeks
- Confirm editing by sequencing and analyze protein loss by Western blot or immunostaining
Troubleshooting:
- Low editing efficiency: Optimize delivery method, test multiple sgRNAs, use hybrid Cas9-D10A nickase
- High cell toxicity: Use RNP delivery instead of plasmids, titrate Cas9 concentration
- Off-target effects: Use computational prediction tools to assess potential off-target sites, employ high-fidelity Cas9 variants
Advanced Genome Editing Technologies
Base Editing and Prime Editing
While standard CRISPR-Cas9 introduces double-strand breaks that activate DNA repair pathways, newer technologies have been developed to enable more precise editing without creating double-strand breaks. Base editing uses a catalytically impaired Cas protein (nickase) fused to a deaminase enzyme to directly convert one DNA base to another without breaking the DNA backbone [4]. Cytosine base editors (CBEs) convert C•G to T•A base pairs, while adenine base editors (ABEs) convert A•T to G•C base pairs [4]. Prime editing represents a further advancement, using a Cas9 nickase fused to a reverse transcriptase and a prime editing guide RNA (pegRNA) that specifies both the target site and contains the desired edit template [5]. This system can mediate all 12 possible base-to-base conversions, as well as small insertions and deletions, without double-strand breaks [4].
Table 2: Comparison of CRISPR Genome Editing Platforms
| Platform | Mechanism | Editing Outcomes | Advantages | Therapeutic Applications |
|---|---|---|---|---|
| CRISPR-Cas9 | Double-strand break + NHEJ/HDR | Indels, precise insertions | High efficiency for gene disruption | Sickle cell disease (Casgevy) [3] |
| Base Editing | Direct chemical conversion | Point mutations | No double-strand breaks, higher precision | VERVE-101/102 for cholesterol reduction [6] |
| Prime Editing | Reverse transcription + pegRNA | Point mutations, small indels | Broad editing scope, minimal byproducts | Preclinical development for various diseases [5] |
| Epigenetic Editing | Catalytically dead Cas + modifiers | Gene expression modulation | Reversible, no sequence alteration | Preclinical studies for gene regulation [7] |
Experimental Protocol: Prime Editing in Human Cells
Protocol Title: Prime Editing for Precise Genome Modification
Principle: Prime editing uses a prime editing guide RNA (pegRNA) to direct a Cas9 nickase-reverse transcriptase fusion protein to the target site, where it nicks the DNA and uses the pegRNA-encoded template for reverse transcription to install desired edits without double-strand breaks.
Materials:
- Prime editor expression plasmid (e.g., PE2, PE3 systems)
- Cells with high HDR efficiency (e.g., HEK293T, HAP1, or iPSCs)
- Transfection reagents optimized for the cell type
- pegRNA design tools (e.g., PrimeDesign)
- PCR reagents and sequencing primers
- Puromycin or other selection agents (if using selection)
Procedure:
pegRNA Design
- Identify edit location and design 13-16 nt primer binding site (PBS)
- Design reverse transcription template (RTT) containing desired edit (typically 10-16 nt)
- Ensure pegRNA spacer has high on-target activity and minimal off-targets
- Optional: Design nicking sgRNA for PE3 system to increase efficiency
Vector Construction
- Clone pegRNA into appropriate expression vector
- Co-transfect with prime editor plasmid or use all-in-one vector
- Include controls: empty vector, pegRNA only
Delivery and Selection
- Transfect cells using recommended method for cell type
- For difficult-to-transfect cells, use nucleofection with RNP complexes
- Apply puromycin selection 24h post-transfection if using selection marker
- Harvest cells at 72h for initial efficiency assessment
Analysis of Editing Efficiency
- Extract genomic DNA from harvested cells
- Amplify target region with high-fidelity polymerase
- Use next-generation sequencing for quantitative assessment
- Calculate efficiency as percentage of reads containing desired edit
Optimization Tips:
- Test multiple pegRNAs with varying PBS and RTT lengths
- For difficult edits, use PE3 system with additional nicking sgRNA
- Employ engineered prime editor variants (PEmax) for enhanced efficiency
- Use mismatch repair inhibitors (e.g., MLH1dn) to improve efficiency in some cell types
Therapeutic Applications and Clinical Trials
The translation of CRISPR technology from basic research to clinical applications has progressed rapidly, with the first FDA-approved therapy arriving in 2023. Casgevy (exa-cel), developed by CRISPR Therapeutics and Vertex Pharmaceuticals, received approval for treating sickle cell disease and transfusion-dependent beta thalassemia [3]. This therapy uses ex vivo editing of autologous CD34+ hematopoietic stem cells to reactivate fetal hemoglobin production, demonstrating the potential of CRISPR-based therapies to address genetic disorders at their root cause.
Current clinical trials are exploring CRISPR applications across diverse disease areas, including genetic disorders, cancers, and infectious diseases. Intellia Therapeutics has pioneered in vivo CRISPR delivery using lipid nanoparticles (LNPs) to target the liver for treating hereditary transthyretin amyloidosis (hATTR) and hereditary angioedema (HAE) [8]. Their Phase I results published in 2024 showed sustained reduction of disease-causing proteins with a single infusion [8]. Notably, the LNP delivery system enables repeat dosing, overcoming a significant limitation of viral vector-based approaches [8].
Table 3: Selected CRISPR-Based Clinical Trials and Therapeutics
| Therapy | Target Condition | Editing Approach | Delivery Method | Development Stage |
|---|---|---|---|---|
| Casgevy | Sickle cell disease, Beta thalassemia | CRISPR-Cas9 (BCL11A enhancer) | Ex vivo (CD34+ cells) | FDA-approved (2023) [3] |
| NTLA-2001 | Transthyretin amyloidosis | CRISPR-Cas9 (TTR knockout) | In vivo (LNP) | Phase III (paused due to adverse event) [7] [6] |
| NTLA-2002 | Hereditary angioedema | CRISPR-Cas9 (KLKB1 knockout) | In vivo (LNP) | Phase I/II (86% kallikrein reduction) [8] |
| VERVE-101 | Heterozygous familial hypercholesterolemia | Base editing (PCSK9 inactivation) | In vivo (LNP) | Phase Ib (paused) [6] |
| FT819 | Systemic lupus erythematosus | CRISPR-Cas9 (CAR-T cells) | Ex vivo (T cells) | Phase I (promising results) [7] |
| CTX310 | Hypercholesterolemia | CRISPR-Cas9 (ANGPTL3 knockout) | In vivo (LNP) | Phase I (updates expected 2025) [6] |
Experimental Protocol: Lipid Nanoparticle-Mediated In Vivo Delivery
Protocol Title: In Vivo Genome Editing Using CRISPR-LNP Formulations
Principle: This protocol describes the formulation of CRISPR-Cas9 components in liver-tropic lipid nanoparticles for in vivo delivery, enabling targeted genome editing in hepatocytes without ex vivo manipulation of cells.
Materials:
- Cas9 mRNA or plasmid DNA
- sgRNA or crRNA and tracrRNA
- Ionizable lipid (e.g., DLin-MC3-DMA, ALC-0315)
- Helper lipids (DSPC, cholesterol, PEG-lipid)
- Microfluidic mixer (e.g., NanoAssemblr)
- Dialysis membranes and cassettes
- Animal model for testing
- Analytical methods for editing assessment
Procedure:
CRISPR Payload Preparation
- For mRNA delivery: Use purified Cas9 mRNA with modified nucleotides (e.g., pseudouridine) for enhanced stability
- For RNP delivery: Complex purified Cas9 protein with sgRNA at 3:1 molar ratio in appropriate buffer
- Confirm integrity and purity of nucleic acids/proteins by electrophoresis and spectrometry
LNP Formulation
- Prepare lipid mixture in ethanol: ionizable lipid, DSPC, cholesterol, PEG-lipid (50:10:38.5:1.5 molar ratio)
- Prepare aqueous phase containing CRISPR payload in citrate buffer (pH 4.0)
- Use microfluidic mixer to combine aqueous and lipid phases at 3:1 flow rate ratio
- Dialyze formed LNPs against PBS (pH 7.4) to remove ethanol and adjust pH
LNP Characterization
- Measure particle size and polydispersity by dynamic light scattering (target: 70-100 nm)
- Determine encapsulation efficiency using RiboGreen assay for RNA (>90% target)
- Assess surface charge by zeta potential measurement
- Examine morphology by transmission electron microscopy
In Vivo Administration and Analysis
- Administer CRISPR-LNPs via intravenous injection in animal model
- For liver targeting, use dose of 0.5-1.0 mg RNA/kg body weight
- Harvest tissues at appropriate timepoints (e.g., 7-14 days post-injection)
- Analyze editing efficiency by next-generation sequencing of target region
- Assess protein-level changes by ELISA or Western blot where applicable
- Monitor potential immune responses and liver toxicity
Notes:
- LNP composition can be adjusted to target different tissues beyond liver
- Include control LNPs with non-targeting sgRNA
- Optimal results achieved with fresh LNP preparations; avoid freeze-thaw cycles
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of CRISPR-based experiments requires careful selection of reagents and optimization of protocols. The table below outlines key materials and their applications in CRISPR research.
Table 4: Essential Research Reagents for CRISPR-Cas9 Experiments
| Reagent Category | Specific Examples | Function/Application | Notes |
|---|---|---|---|
| Cas9 Expression Systems | SpCas9, SaCas9, Cas12a, HiFi Cas9 | DNA cleavage with varying PAM requirements, sizes | HiFi variants reduce off-target effects [9] |
| Delivery Vehicles | AAV vectors, Lentivirus, LNPs, Electroporation | Introduction of editing components into cells | AAV limited by packaging size; LNPs enable repeat dosing [8] |
| sgRNA Synthesis | In vitro transcription, Chemical synthesis, Cloned vectors | Target sequence specification | Chemical synthesis allows for extensive modifications |
| Editing Enhancers | Alt-R HDR Enhancer, Rad51 agonists | Increase HDR efficiency for precise edits | Alt-R HDR Enhancer improves efficiency 2-fold in stem cells [5] |
| Detection Tools | T7E1, TIDE, NGS, Digital PCR | Assessment of editing efficiency and specificity | NGS provides most comprehensive analysis |
| Cell Culture | Stem cell media, Cytokines, Matrices | Maintenance and expansion of target cells | Critical for primary and stem cell applications |
| Control Reagents | Non-targeting sgRNAs, Fluorescent reporters | Experimental validation and optimization | Essential for distinguishing specific from non-specific effects |
| ZG297 | ZG297, MF:C31H35F3N4O3, MW:568.6 g/mol | Chemical Reagent | Bench Chemicals |
| HKI12134085 | HKI12134085, MF:C18H18F3N3O5S, MW:445.4 g/mol | Chemical Reagent | Bench Chemicals |
Diagram 2: Therapeutic CRISPR Development Workflow. This diagram outlines the key decision points and processes in developing CRISPR-based therapies, from target identification to clinical application.
The evolution of CRISPR technology continues at a rapid pace, with several emerging trends shaping its future applications in therapeutic cell design. Artificial intelligence is now being employed to design novel CRISPR systems, as demonstrated by the recent development of OpenCRISPR-1, an AI-generated editor that shows comparable activity to SpCas9 despite being 400 mutations distant in sequence [9]. Delivery technologies represent another frontier, with ongoing efforts to develop LNPs that target organs beyond the liver and improve the safety profile of in vivo editing [8]. Additionally, epigenetic editing approaches using catalytically dead Cas proteins fused to epigenetic modifiers offer the potential for reversible gene regulation without permanent DNA changes [7].
The clinical landscape for CRISPR therapies is expanding beyond monogenic disorders to include common conditions such as cardiovascular disease, with multiple candidates in development for cholesterol management [6]. The successful administration of the first personalized in vivo CRISPR therapy to an infant with CPS1 deficiency in 2025 demonstrates the potential for rapid development of bespoke treatments for rare genetic disorders [8]. However, challenges remain, including the recent pause in Intellia's Phase III trial due to a serious adverse event, highlighting the importance of continued safety evaluation [7].
For researchers and drug development professionals, the CRISPR toolkit has expanded dramatically, offering multiple platforms for different therapeutic applications. The choice between conventional CRISPR-Cas9, base editing, prime editing, or epigenetic approaches depends on the specific genetic modification required, the target cell type, and the desired permanence of the intervention. As the field progresses, the integration of AI-designed editors, improved delivery systems, and enhanced safety profiling will likely unlock new therapeutic possibilities, ultimately fulfilling the promise of precision genetic medicine across a broad spectrum of human diseases.
The CRISPR-Cas9 system has revolutionized therapeutic cell design by providing an unprecedented ability to make precise, targeted changes to the genome of living cells. Derived from a bacterial adaptive immune system, this technology enables researchers to permanently modify gene function with high efficiency and relative ease compared to previous technologies like zinc finger nucleases (ZFNs) and transcription activator-like effector nucleases (TALENs) [10]. For researchers and drug development professionals, understanding the core molecular mechanisms—guide RNA design, Cas9 nuclease function, and Protospacer Adjacent Motif (PAM) requirements—is fundamental to developing safe and effective cell-based therapies. This protocol details the experimental approaches for leveraging these mechanisms within therapeutic development workflows.
The fundamental CRISPR-Cas9 machinery consists of two key components: the Cas9 nuclease, which creates double-stranded breaks in DNA, and a guide RNA (gRNA), which directs Cas9 to a specific genomic location [10]. Target recognition is initiated by the binding of a short DNA sequence known as the Protospacer Adjacent Motif (PAM) to a groove formed by Cas9's C-terminal region [11]. This PAM interaction enables the guide RNA to hybridize with the target DNA strand, leading to DNA cleavage and subsequent repair by cellular mechanisms [12].
Diagram: Core CRISPR-Cas9 Mechanism in Therapeutic Cell Design
Guide RNA (gRNA) Design: Principles and Protocols
The guide RNA is a synthetic RNA composed of a CRISPR RNA (crRNA) trans-activating crRNA (tracrRNA) fusion that directs Cas9 to a specific DNA target sequence through complementary base pairing [10]. A well-designed gRNA is the most critical factor for achieving high on-target efficiency while minimizing off-target effects.
Fundamental Design Rules
The gRNA contains a 20-nucleotide spacer sequence that is complementary to the target DNA site. This target site must be located immediately adjacent to a PAM sequence that is recognized by the specific Cas nuclease being used [13]. For the most commonly used Streptococcus pyogenes Cas9 (SpCas9), the PAM sequence is 5'-NGG-3', located immediately 3' of the target sequence [10]. The gRNA spacer sequence should be designed to have perfect complementarity to the genomic target, and its positioning should consider the type of edit to be made. For gene knockouts via non-homologous end joining (NHEJ), the spacer should target early exons to maximize the probability of generating frameshift mutations. For homology-directed repair (HDR), the spacer should place the cut site as close as possible to the intended edit.
Protocol: Designing and Validating gRNAs for Therapeutic Targets
Materials:
- Genomic DNA sequence of target gene
- CRISPR gRNA design software (e.g., CRISPR Design Tool, ZiFiT Targeter)
- Oligonucleotides for gRNA cloning
- gRNA expression vector (e.g., pX330 or similar)
- Target cell line
- Genomic DNA extraction kit
- T7 Endonuclease I or next-generation sequencing platform for validation
Procedure:
Target Identification:
- Input the genomic sequence of your target region into a gRNA design tool.
- Identify all potential 20-nucleotide sequences followed by a 5'-NGG-3' PAM (for SpCas9) on both DNA strands.
- Cross-reference potential gRNA sequences with databases of known genetic variants to avoid polymorphisms.
Specificity Screening:
- Use the design tool to identify potential off-target sites with up to 5 nucleotide mismatches [10].
- Prioritize gRNAs with minimal homology to other genomic regions, especially those with 3 or more consecutive mismatches in the "seed" region proximal to the PAM.
- For therapeutic applications, select 3-5 candidate gRNAs for empirical testing.
gRNA Construction:
- Synthesize oligonucleotides corresponding to the selected spacer sequences with appropriate overhangs for your chosen expression system.
- Anneal and clone oligonucleotides into the gRNA expression vector according to standard molecular biology protocols.
- Verify constructs by Sanger sequencing.
Efficiency Validation:
- Transfect target cells with your Cas9/gRNA constructs using an appropriate method for your cell type.
- After 48-72 hours, harvest genomic DNA and amplify the target region by PCR.
- Assess editing efficiency using the T7 Endonuclease I assay [10] or next-generation sequencing.
- Select the gRNA with the highest on-target efficiency and lowest off-target activity for therapeutic development.
Table 1: Troubleshooting Guide for gRNA Design and Validation
| Problem | Potential Cause | Solution |
|---|---|---|
| Low editing efficiency | Poor gRNA binding affinity | Redesign gRNA with different target site; check GC content (40-60% optimal) |
| High off-target activity | gRNA sequence has high similarity to non-target sites | Use truncated gRNAs (17-18 nt) [10] or select alternative gRNA with lower homology to other genomic regions |
| No detectable editing | PAM not functional in chromatin context | Verify PAM availability using chromatin accessibility data; try different gRNA targeting same region |
| Inconsistent results between replicates | Variable transfection efficiency | Include a fluorescent reporter to monitor efficiency; use stable cell lines for Cas9 expression |
Cas9 Nuclease Function: Mechanism and Engineering
The Cas9 nuclease functions as a molecular scalpel that creates precise double-stranded breaks (DSBs) in DNA at locations specified by the gRNA. Understanding its mechanism is essential for selecting the appropriate variant for therapeutic applications.
Molecular Mechanism of DNA Cleavage
Cas9 undergoes a conformational change upon forming a complex with the gRNA, enabling it to interrogate DNA sequences for PAM recognition [11]. Once a PAM is bound, the protein unwinds the adjacent DNA, allowing the gRNA to form an RNA-DNA heteroduplex with its target sequence. Successful complementarity between the gRNA and target DNA activates Cas9's two nuclease domains: the HNH domain cleaves the DNA strand complementary to the gRNA (target strand), while the RuvC-like domain cleaves the opposite strand (non-target strand) [10]. This coordinated activity results in a blunt-ended, double-stranded break approximately 3-4 nucleotides upstream of the PAM sequence.
Engineered Cas9 Variants for Enhanced Therapeutic Applications
Different Cas9 variants offer unique properties suited to specific therapeutic applications:
Cas9D10A (Nickase): This variant contains a point mutation in the RuvC domain that cleaves only the non-target strand, creating single-strand breaks or "nicks" [10]. Using two adjacent nickase complexes (paired nickases) increases specificity by requiring simultaneous binding at both sites to create a functional double-strand break, significantly reducing off-target effects [10].
dCas9 (Nuclease-deficient): Mutations in both catalytic domains (D10A in RuvC and H840A in HNH) completely inactivate cleavage activity while preserving DNA binding capability [10]. When fused to effector domains, dCas9 can be used for precise transcriptional control (CRISPRa/i), epigenetic modification, or genomic labeling without altering the DNA sequence—particularly valuable for functional genomics in therapeutic cell design.
High-Fidelity Variants: Engineered Cas9 variants such as Alt-R S.p. HiFi Cas9 nuclease have been specifically modified to dramatically reduce off-target editing while maintaining high on-target activity [14]. These variants are particularly important for therapeutic applications where specificity is paramount.
Table 2: Cas9 Nuclease Variants and Their Applications in Therapeutic Cell Design
| Cas9 Variant | Key Mutations | Cleavage Activity | Primary Therapeutic Applications |
|---|---|---|---|
| Wild-Type SpCas9 | None | DSB | Gene knockout, gene insertion (with donor template) |
| Cas9D10A (Nickase) | D10A in RuvC domain | SSB (nicks one strand) | Paired nicking for enhanced specificity, HDR with reduced NHEJ |
| dCas9 | D10A + H840A | Catalytically inactive | Gene regulation (CRISPRa/i), epigenetic editing, live imaging |
| Cas9-HF1 | N497A, R661A, Q695A, Q926A | DSB with reduced off-targets | Therapeutic applications requiring high specificity |
| HiFi Cas9 | R691A | DSB with minimal off-targets | Clinical therapeutic development |
PAM Requirements: Characterization and Engineering
The Protospacer Adjacent Motif (PAM) is a short, specific DNA sequence adjacent to the target site that Cas9 requires for target recognition. PAM sequences act as a signal for Cas nucleases, indicating they have found the correct modification site [14]. The PAM requirement is both a fundamental constraint and a safety feature that prevents unintended cleavage of the CRISPR array in native bacterial systems.
Natural PAM Diversity Across Cas Orthologs
Different Cas nucleases recognize distinct PAM sequences, providing a natural toolkit for targeting different genomic regions:
Table 3: PAM Requirements of Commonly Used Cas Nucleases
| Cas Nuclease | Source Organism | PAM Sequence (5'→3') | Notes on Targeting Range |
|---|---|---|---|
| SpCas9 | Streptococcus pyogenes | NGG | Most widely used; requires G-rich PAM |
| SaCas9 | Staphylococcus aureus | NNGRRT | More restrictive PAM; smaller size for delivery |
| CjCas9 | Campylobacter jejuni | NNNNACAC | Extended PAM sequence; unique targeting |
| AsCas12a | Acidaminococcus sp. | TTTV | T-rich PAM; creates staggered cuts |
| LbCas12a | Lachnospiraceae bacterium | TTTV | Similar to AsCas12a with variations |
| AsCas12f1 | Acidaminococcus sp. | NTTR | Ultra-small size; emerging therapeutic potential |
| PlmCas12e | Uncultured archaeon | TTCN | Compact size with simple PAM |
Protocol: Determining PAM Requirements with GenomePAM
Traditional methods for PAM characterization require laborious protein purification and in vitro cleavage assays. The recently developed GenomePAM method enables direct PAM characterization in mammalian cells by leveraging genomic repetitive sequences as naturally occurring target sites, eliminating the need for protein purification or synthetic oligo libraries [15].
Materials:
- Mammalian cell line (e.g., HEK293T)
- Candidate Cas nuclease expression plasmid
- gRNA expression vector targeting repetitive sequence (e.g., Rep-1: 5'-GTGAGCCACTGTGCCTGGCC-3')
- GUIDE-seq reagents [15]
- Next-generation sequencing platform
- Bioinformatics tools for sequence analysis
Procedure:
Guide RNA Design:
- For type II Cas nucleases with 3' PAMs (e.g., SpCas9, SaCas9), use Rep-1 as the protospacer sequence.
- For type V Cas nucleases with 5' PAMs (e.g., FnCas12a), use the reverse complement Rep-1RC (5'-GGCCAGGCACAGTGGCTCAC-3') as the protospacer [15].
- Clone the appropriate spacer into your gRNA expression vector.
Cell Transfection and GUIDE-seq:
- Co-transfect HEK293T cells with your candidate Cas nuclease plasmid and the Rep-1 gRNA vector.
- Simultaneously introduce the GUIDE-seq dsODN tag using optimized transfection protocols [15].
- Culture cells for 72 hours to allow for genome editing and tag integration.
Sequencing and Data Analysis:
- Harvest genomic DNA and perform GUIDE-seq library preparation using anchor multiplex PCR sequencing (AMP-seq) [15].
- Sequence the resulting libraries on an appropriate next-generation sequencing platform.
- Align sequences to the reference genome and identify cleavage sites through detection of integrated dsODN tags.
PAM Identification:
- Extract the flanking sequences (typically 10 bp) from all identified cleavage sites.
- Use the iterative "seed-extension" method to identify statistically significant enriched motifs [15].
- Generate sequence logos and calculate relative PAM cleavage values (PCVs) to quantify preference strength.
- Validate the identified PAM requirements through targeted editing assays with synthetic constructs.
Diagram: GenomePAM Workflow for PAM Characterization
PAM Engineering for Expanded Targeting Scope
Protein engineering approaches have created Cas9 variants with altered PAM specificities to overcome the targeting limitations of wild-type nucleases:
VQR Variant: (D1135V, R1335Q, T1337R) recognizes 5'-NGA-3' PAMs [11] VRER Variant: (D1135V, G1218R, R1335E, T1337R) recognizes 5'-NGCG-3' PAMs [11] EQR Variant: (D1135E, R1335Q, T1337R) recognizes 5'-NGAG-3' PAMs [11] SpRY: Near-PAMless variant that recognizes 5'-NRN-3' > 5'-NYN-3' [15]
These engineered variants employ a combination of direct PAM-interacting residue mutations and distal allosteric mutations (e.g., D1135V) that stabilize the PAM-binding domain and preserve long-range communication with the REC3 domain, which relays signals to the HNH nuclease [11]. This expanded PAM compatibility significantly increases the number of targetable sites in the human genome for therapeutic applications.
The Scientist's Toolkit: Essential Reagents for CRISPR-based Therapeutic Cell Design
Table 4: Key Research Reagent Solutions for CRISPR-Cas9 Experiments
| Reagent/Category | Function/Description | Example Products/Notes |
|---|---|---|
| Cas9 Nuclease Variants | Catalytic component for DNA cleavage | Wild-type SpCas9, HiFi Cas9 (reduced off-target), Cas9D10A (nickase), dCas9 (catalytically inactive) |
| gRNA Expression Systems | Delivery of targeting component | U6-driven vectors, chemically modified synthetic gRNAs (enhanced stability) |
| Delivery Vehicles | Introduction of editing components into cells | Lipid nanoparticles (LNP) [8], adeno-associated viruses (AAV), electroporation systems |
| PAM Characterization Tools | Determination of nuclease targeting requirements | GenomePAM system [15], HT-PAMDA, PAM-SCANR |
| Editing Detection Assays | Validation of editing efficiency and specificity | T7 Endonuclease I mismatch assay, next-generation sequencing, GUIDE-seq [15] |
| Bioinformatics Tools | gRNA design and off-target prediction | CRISPR Design Tool, ZiFiT Targeter, Cas-OFFinder |
| Cell Culture Resources | Maintenance and expansion of target cells | Appropriate media, cell lines, primary cell culture reagents |
| HDR Donor Templates | Precision genome editing with template-directed repair | Single-stranded oligodeoxynucleotides (ssODNs), double-stranded DNA donors with homology arms |
| Ebv ebna3A (379-387) | Ebv ebna3A (379-387), MF:C55H94N18O10, MW:1167.5 g/mol | Chemical Reagent |
| Isookanin | Isookanin, CAS:1036-49-3, MF:C15H12O6, MW:288.25 g/mol | Chemical Reagent |
The CRISPR-Cas9 system has revolutionized genetic research by providing unprecedented precision in genome editing. However, the CRISPR-Cas9 enzyme functions merely as "molecular scissors" that create targeted double-strand breaks (DSBs) in DNA [16]. The actual genetic modifications occur through the cell's endogenous DNA Damage Repair (DDR) pathways, which are activated to repair these breaks [16]. Two principal pathways—Non-Homologous End Joining (NHEJ) and Homology-Directed Repair (HDR—compete to repair DSBs, each resulting in distinct genetic outcomes [16] [17]. Understanding and controlling these pathways is fundamental to therapeutic cell design, enabling researchers to pursue either gene disruption or precise correction strategies.
NHEJ represents a "quick-fix" repair mechanism that directly ligates broken DNA ends without requiring a template [16]. This pathway is active throughout the cell cycle and predominates in most cells due to its speed [16] [18]. However, this efficiency comes at the cost of precision, as NHEJ often results in small insertions or deletions (indels) at the repair site [16] [19]. In therapeutic contexts, researchers harness this propensity for indels to disrupt gene function, making NHEJ ideal for generating gene knockouts [16] [20].
In contrast, HDR is a precise repair mechanism that requires a homologous DNA template to faithfully restore the original sequence or incorporate designed changes [16] [17]. This pathway is restricted to the S and G2 phases of the cell cycle when homologous DNA is naturally available [16]. In CRISPR editing, researchers supply an exogenous donor template containing the desired modification flanked by homology arms, enabling precise gene correction or knock-in [17] [19]. While HDR offers unparalleled accuracy, its lower efficiency relative to NHEJ presents a significant challenge for therapeutic applications [17] [21].
Quantitative Comparison of NHEJ and HDR
Table 1: Key Characteristics of NHEJ and HDR Repair Pathways
| Parameter | Non-Homologous End Joining (NHEJ) | Homology-Directed Repair (HDR) |
|---|---|---|
| Template Requirement | No homologous template needed [16] | Requires homologous template (donor DNA) [16] [17] |
| Cell Cycle Phase | Active throughout all phases [16] [18] | Primarily restricted to S and G2 phases [16] |
| Repair Speed | Fast (repair half-life: 1-10 hours) [18] | Slower process [16] |
| Efficiency | High efficiency in most cell types [16] | Low efficiency compared to NHEJ [17] [21] |
| Fidelity | Error-prone, generates indels [16] [19] | High precision, accurate repair [16] [17] |
| Primary Applications | Gene knockouts, gene disruption [16] [22] | Point mutations, gene correction, knock-ins [16] [17] |
| Key Proteins | Ku70/Ku80, DNA-PKcs, XRCC4, DNA Ligase IV [17] | RAD51, BRCA2, PALB2 [17] |
Table 2: HDR Efficiency Optimization Strategies
| Strategy | Method | Reported Outcome |
|---|---|---|
| NHEJ Inhibition | Small molecule inhibitors (e.g., DNA-PKcs inhibitors) [17] [21] | Increases HDR efficiency by reducing competing repair pathway [21] |
| MMEJ Inhibition | POLQ knockout or inhibition [21] | Further increases HDR proportion by eliminating backup repair pathway [21] |
| Combined Inhibition | HDRobust approach: simultaneous NHEJ and MMEJ inhibition [21] | Achieves HDR in up to 93% of chromosomes with minimal indels [21] |
| Cell Synchronization | Arrest cells in S/G2 phase [17] | Increases proportion of cells competent for HDR [17] |
| Donor Design | Single-stranded oligodeoxynucleotides (ssODNs) with optimized homology arms [19] | Improves HDR efficiency through enhanced donor accessibility [19] |
Protocol for NHEJ-Mediated Gene Knockout
Experimental Workflow for Gene Disruption
Detailed Methodology
Step 1: Guide RNA Design and Validation
- Design sgRNAs targeting early exons of the gene of interest to maximize likelihood of functional disruption [22]. Avoid targeting regions close to the N- or C-terminus, as alternative start codons or non-essential protein domains may preserve function [22].
- Select sgRNAs with high on-target activity scores using validated algorithms (e.g., Doench rules) [22] [23]. For critical applications, design multiple sgRNAs (typically 2-3) targeting the same gene to improve knockout efficiency [22].
- Validate sgRNA specificity using off-target prediction tools to minimize unintended genomic alterations [23].
Step 2: Delivery of CRISPR Components
- Prepare CRISPR-Cas9 ribonucleoprotein (RNP) complexes by pre-assembling purified Cas9 protein with synthetic sgRNA at molar ratios between 1:1 and 1:3 (Cas9:sgRNA) [23].
- Deliver RNP complexes to target cells via electroporation for immune cells or lipid-based transfection for adherent cell lines [19]. For primary cells or difficult-to-transfect cells, consider viral delivery systems (lentivirus, AAV) with optimized titers [19] [18].
- For in vivo applications, utilize lipid nanoparticles (LNPs) optimized for target tissue tropism [24] [8].
Step 3: Validation and Screening
- Harvest cells 72-96 hours post-delivery and extract genomic DNA using standard protocols.
- Amplify target region by PCR using primers flanking the cut site (typically 300-500 bp amplicon size).
- Analyze indels by tracking of indels by decomposition (TIDE) or next-generation sequencing to quantify knockout efficiency [18].
- For clonal analysis, single-cell sort edited cells and expand for 2-3 weeks before validating knockout via Western blot or functional assays.
Protocol for HDR-Mediated Precise Editing
Experimental Workflow for Precise Correction
Detailed Methodology
Step 1: Donor Template and sgRNA Design
- Design single-stranded oligodeoxynucleotides (ssODNs) as donor templates for point mutations or small insertions (<200 bp). For larger insertions, use double-stranded DNA plasmids with homology arms [19].
- For ssODNs, incorporate silent mutations (blocking mutations) in the PAM sequence or seed region to prevent Cas9 re-cleavage after successful editing [21].
- Position the cut site as close as possible to the intended edit (typically within 10 bp or less) for optimal HDR efficiency [16] [22].
- For ssODNs, use homology arms of 30-90 nucleotides on each side, with total length not exceeding 200 nucleotides [19]. For plasmid donors, use 500-1000 bp homology arms.
Step 2: HDR Optimization Strategies
- Synchronize cells in S/G2 phase where HDR is most active using cell cycle inhibitors such as nocodazole or aphidicolin [17].
- Inhibit the NHEJ pathway using small molecule inhibitors such as NU7026 (DNA-PKcs inhibitor) or SCR7 (DNA Ligase IV inhibitor) during the first 24-48 hours after editing [17] [21].
- Implement the HDRobust approach by simultaneously inhibiting NHEJ and MMEJ pathways through combined treatment with DNA-PKcs and Polθ inhibitors [21].
- For in vivo applications, consider LNP formulations that enable redosing to increase the proportion of edited cells, as demonstrated in clinical trials [8].
Step 3: Delivery and Validation
- Co-deliver CRISPR components and donor templates at optimal ratios. For RNP delivery, maintain Cas9:sgRNA:donor molar ratios between 1:1:5 and 1:1:10 [21].
- For difficult-to-edit cell types (e.g., neurons, cardiomyocytes), consider virus-like particles (VLPs) for efficient RNP delivery [18].
- Allow 7-14 days for complete repair in slow-dividing or postmitotic cells, as HDR efficiency continues to increase over this period [18].
- Validate precise editing using a combination of restriction fragment length polymorphism (RFLP) analysis, Sanger sequencing, and digital PCR. Always screen for potential off-target effects at predicted sites [23].
DNA Repair Pathway Diagram
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Research Reagent Solutions for CRISPR Genome Editing
| Reagent Category | Specific Examples | Function and Application Notes |
|---|---|---|
| CRISPR Nucleases | Wild-type SpCas9, Cas9-HiFi, Cas12a (Cpf1) [23] | Generate DSBs at target sites. HiFi variants reduce off-target effects [23]. |
| Guide RNA Formats | Synthetic sgRNA, crRNA:tracrRNA complexes [22] [23] | Direct Cas nuclease to target sequence. Synthetic sgRNAs offer high consistency [22]. |
| Donor Templates | Single-stranded ODNs (ssODNs), double-stranded DNA plasmids with homology arms [19] | Provide repair template for HDR. ssODNs ideal for point mutations, plasmids for large insertions [19]. |
| Delivery Systems | Electroporation, lipid nanoparticles (LNPs), virus-like particles (VLPs), AAV [19] [18] [8] | Introduce editing components into cells. LNPs preferred for in vivo liver targeting [8]. |
| NHEJ Inhibitors | NU7026, KU0060648 (DNA-PKcs inhibitors) [17] [21] | Enhance HDR efficiency by suppressing competing NHEJ pathway [21]. |
| MMEJ Inhibitors | Polθ inhibitors [21] | Further improve HDR efficiency by blocking microhomology-mediated end joining [21]. |
| Validation Tools | TIDE decomposition, next-generation sequencing, digital PCR [18] | Quantify editing efficiency and detect off-target effects [18] [23]. |
| Herbarin | Herbarin, MF:C16H16O6, MW:304.29 g/mol | Chemical Reagent |
| Dotriacolide | Dotriacolide, MF:C40H76O18S4, MW:973.3 g/mol | Chemical Reagent |
The CRISPR-Cas adaptive immune system, inherent in bacteria and archaea, has been repurposed as a revolutionary biotechnology toolset. While CRISPR-Cas9 has been the most widely adopted system, the CRISPR landscape is remarkably diverse, encompassing two primary classes based on effector module architecture. Class 1 (Types I, III, IV, and VII) utilizes multi-subunit effector complexes, whereas Class 2 (Types II, V, and VI) employs single effector proteins, making them particularly suitable for biotechnological applications [25] [26]. The rapid discovery and characterization of new Cas effectors beyond Cas9—including Cas12, Cas13, Cas14, and other rare variants—are continuously expanding the capabilities and applications of genome engineering, diagnostics, and therapeutic design [25] [27] [28]. This document details the mechanisms, applications, and experimental protocols for these alternative systems within the context of therapeutic cell design research.
Cas12 Systems: Mechanisms and Applications
Molecular Mechanism and Types
Cas12 is a Class 2, Type V effector that targets and cleaves DNA. Unlike Cas9, which requires two RNA molecules (crRNA and tracrRNA), most Cas12 systems (e.g., Cas12a/Cpf1) utilize a single crRNA for guidance and possess a single RuvC-like nuclease domain that cleaves both strands of DNA, generating staggered ends with 5' overhangs [26] [28]. A key diagnostic feature of many Cas12 proteins is their collateral activity; upon recognizing and cleaving its target DNA, the Cas12 nuclease becomes activated to non-specifically degrade any nearby single-stranded DNA (ssDNA) [29]. This property is the foundation for several sensitive diagnostic tools. Variants like Cas12b and the ultra-compact Cas12f have also been identified and engineered for use in plant and mammalian cells, with Cas12f being of particular interest for therapeutic delivery due to its small size [28].
Applications in Therapeutic Cell Design
Cas12 systems are versatile tools for cell engineering:
- Gene Disruption: Efficient gene knockout in primary T-cells and hematopoietic stem cells (HSCs) via the non-homologous end joining (NHEJ) repair pathway [4].
- Therapeutic Gene Insertion: The staggered double-strand breaks generated by Cas12a can enhance homology-directed repair (HDR), facilitating the precise insertion of therapeutic transgenes, such as chimeric antigen receptor (CAR) genes into T-cells for cancer immunotherapy [26].
- In Vivo Gene Therapy: The small size of variants like Cas12f and engineered Cas12f1Super (with up to 11-fold improved efficiency) allows for packaging into adeno-associated virus (AAV) vectors for in vivo delivery, enabling direct genome editing within the patient [7].
Table 1: Comparison of Key DNA-Targeting Class 2 Effectors
| Feature | Cas9 | Cas12a (Cpf1) | Cas12f |
|---|---|---|---|
| Class/Type | Class 2, Type II | Class 2, Type V | Class 2, Type V |
| Guide RNA | crRNA + tracrRNA (or sgRNA) | Single crRNA | Single crRNA |
| Cleavage | Blunt ends (typically) | Staggered ends with 5' overhangs | Staggered ends |
| PAM Sequence | 3'-NGG (for SpCas9) | 5'-TTTV (for LbCas12a) | T-rich |
| Collateral Activity | No | Yes (ssDNA degradation) | Yes |
| Protein Size | ~1360 amino acids | ~1300 amino acids | ~400-500 amino acids |
Detailed Protocol: Cas12a-Mediated Gene Insertion in Primary T-Cells
This protocol enables the knock-in of a CAR cassette into the TRAC locus of human T-cells.
Research Reagent Solutions:
- Nucleofector System: For high-efficiency transfection of primary T-cells.
- Cas12a Nuclease: Recombinant LbCas12a or AsCas12a protein.
- crRNA: Designed to target the desired locus (e.g., TRAC). Resuspend in nuclease-free buffer to 100 µM.
- ssODM or AAV Donor Template: Single-stranded oligodeoxynucleotide or AAV vector containing the CAR construct flanked by homology arms to the target locus.
- T-cell Culture Media: X-VIVO 15 medium supplemented with 5% human AB serum and 300 IU/mL IL-2.
- Magnetic Bead Activation Kits: CD3/CD28 beads for T-cell activation.
Methodology:
- Isolation and Activation: Isolate CD3+ T-cells from leukapheresis product using Ficoll density gradient and negative selection. Activate cells with CD3/CD28 activation beads for 24-48 hours in T-cell culture media.
- Ribonucleoprotein (RNP) Complex Formation: Pre-complex 10 µg of Cas12a protein with a 1.5x molar ratio of crRNA. Incubate at room temperature for 10-20 minutes to form the RNP complex.
- Electroporation: Combine the RNP complex with 1-2 million activated T-cells and 2-5 µg of ssODM donor template. Electroporate using a 4D-Nucleofector system with the appropriate T-cell specific program (e.g., EO-115).
- Post-Transfection Culture: Immediately transfer cells to pre-warmed culture media. Remove activation beads 24 hours post-electroporation. Expand cells for 7-14 days, maintaining a density of 0.5-1.5 x 10^6 cells/mL.
- Analysis: Assess editing efficiency 72 hours post-editing via flow cytometry (for surface CAR expression) and genomic DNA extraction followed by next-generation sequencing (NGS) of the target locus to confirm precise integration.
The workflow for this protocol is illustrated below:
Cas13 Systems: Mechanisms and Applications
Molecular Mechanism and Types
Cas13 is a Class 2, Type VI RNA-guided RNA nuclease. Unlike Cas9 and Cas12, which target DNA, Cas13 proteins (e.g., Cas13a, Cas13b, Cas13d) specifically bind and cleave single-stranded RNA (ssRNA) sequences [27] [26]. Similar to Cas12, activated Cas13 exhibits promiscuous collateral RNase activity, cleaving non-target RNA molecules in the vicinity. This property has been harnessed for highly sensitive RNA detection platforms [29]. The ability to target RNA without altering the genome makes Cas13 an attractive tool for transient therapeutic interventions, diagnostics, and basic research.
Applications in Therapeutic Cell Design and Diagnostics
- RNA Knockdown: For transient, reversible gene silencing without permanent genomic changes. This is useful for modulating T-cell differentiation or function in cell therapies, such as knocking down checkpoint inhibitors like PD-1 [28].
- Diagnostics: The collateral activity of Cas13 is the engine behind the SHERLOCK diagnostic platform. It allows for attomolar-sensitive detection of specific RNA pathogens (e.g., SARS-CoV-2) or cellular transcripts, which can be used for quality control of engineered cell products [27] [29].
- Epitranscriptome Editing: Engineered catalytically inactive versions of Cas13 (dCas13) can be fused to various effector domains (e.g., ADAR for A-to-I base editing) to manipulate RNA modifications, offering a new layer of control over gene expression in therapeutic cells [7].
Table 2: Comparison of Key RNA-Targeting and Emerging Cas Effectors
| Feature | Cas13 | Cas14 | Cas7-11 |
|---|---|---|---|
| Class/Type | Class 2, Type VI | Class 2, Type ? (putative) | Class 1, Type III-E |
| Target | Single-stranded RNA (ssRNA) | Single-stranded DNA (ssDNA) | Single-stranded RNA (ssRNA) |
| Collateral Activity | Yes (ssRNA degradation) | Reported | No |
| Primary Application | RNA knockdown, diagnostics | Diagnostics, particularly for ssDNA viruses/phages | Therapeutic RNA editing\n(with reduced collateral activity) |
| Size | ~950-1300 amino acids | Compact (~400-700 amino acids) | Multi-subunit complex |
Detailed Protocol: Cas13d-Mediated mRNA Knockdown in CAR-T Cells
This protocol uses the compact Cas13d ortholog to transiently knock down an endogenous gene (e.g., PDCD1) in CAR-T cells to enhance anti-tumor potency.
Research Reagent Solutions:
- Cas13d Expression Plasmid or mRNA: For in vitro transcription of Cas13d mRNA or a plasmid construct.
- crRNA Expression Cassette: A DNA template or synthetic crRNA targeting the PDCD1 mRNA transcript.
- Lipid Nanoparticles (LNPs) or Electroporation System: For delivery of RNP or mRNA/crRNA.
- qRT-PCR Reagents: For quantifying mRNA knockdown efficiency.
- Flow Cytometry Antibodies: For detecting PD-1 surface protein expression.
Methodology:
- Design and Synthesis: Design a crRNA targeting a conserved region in the PDCD1 mRNA. Synthesize the crRNA chemically or via in vitro transcription. If using mRNA, produce high-quality, capped, and polyadenylated Cas13d mRNA.
- Delivery: For RNP delivery, pre-complex 10 µg of recombinant Cas13d protein with a 3x molar ratio of synthetic crRNA. For mRNA delivery, mix 5 µg of Cas13d mRNA with an equimolar amount of crRNA. Introduce the complexes into pre-activated CAR-T cells via electroporation.
- Incubation and Analysis: Culture the transfected cells for 48-72 hours.
- Harvest cell pellets for RNA extraction and subsequent qRT-PCR analysis to quantify PDCD1 mRNA levels relative to a housekeeping gene (e.g., GAPDH).
- Harvest other cells for flow cytometry to assess the reduction of PD-1 protein on the cell surface.
- Functional Assay: Perform a co-culture assay with target tumor cells to evaluate the functional impact of PD-1 knockdown on CAR-T cell cytokine production and cytotoxic activity.
The logical relationship of this knockdown and analysis workflow is as follows:
Emerging and Engineered Cas Variants
The CRISPR toolbox is continually expanding with the discovery of novel natural systems and the engineering of enhanced variants.
Cas14 and Type VII Systems
Cas14 is a compact, DNA-targeting system found in archaea that uniquely targets single-stranded DNA (ssDNA), making it highly valuable for diagnostic applications against ssDNA viruses and viroids [27]. Type VII systems (e.g., Cas7) are Class 1 systems that target RNA in a crRNA-dependent manner using a β-CASP effector nuclease. They are structurally related to Type III systems but appear to have undergone reductive evolution [25].
Engineered and Compact Variants for Therapy
- Cas7-11: An engineered, single-effector Class 1 system derived from a Type III-E locus. It cleaves target RNA with high specificity and, crucially, lacks robust collateral activity, making it a safer potential alternative to Cas13 for therapeutic RNA editing in human cells [28].
- CasMINI: A hyper-compact Cas protein (about half the size of Cas9 and Cas12a) engineered from Cas12f. Its small size is ideal for delivery via AAV vectors, overcoming a major bottleneck in gene therapy [28].
- SuperFi-Cas9: An engineered version of Cas9 with dramatically improved fidelity, reducing off-target editing by over 4,000-fold without compromising on-target efficiency, thereby addressing a key safety concern for therapeutics [28].
- Prime Editors and PASTE: These are not new Cas proteins but are sophisticated systems built upon Cas9 nickase (H840A). Prime editing uses a Cas9 nickase-reverse transcriptase fusion and a prime editing guide RNA (pegRNA) to directly write new genetic information into a target site without requiring double-strand breaks or donor templates [4] [28]. PASTE further integrates a serine integrase to enable the insertion of large DNA fragments (up to ~36 kb) with high efficiency and minimal off-target effects [28].
The Scientist's Toolkit: Essential Reagents and Solutions
Table 3: Key Research Reagent Solutions for CRISPR Cell Engineering
| Reagent/Solution | Function | Example Use-Case |
|---|---|---|
| GMP-grade gRNAs & Nucleases | Ensures purity, safety, and efficacy for clinical development. Critical for regulatory approval [30]. | Manufacturing a CRISPR-based therapy for clinical trials. |
| Lipid Nanoparticles (LNPs) | In vivo delivery vehicle for CRISPR components (mRNA, gRNA). Particularly effective for targeting the liver [8]. | Systemic administration of CRISPR-LNP therapy for hereditary transthyretin amyloidosis (hATTR). |
| AAV Vectors | In vivo delivery vehicle for CRISPR machinery. Serotype determines tropism. Size constrained (~4.7 kb). | Delivering compact editors like CasMINI or Cas12f for in vivo gene editing. |
| Nucleofector Systems | High-efficiency electroporation platform for hard-to-transfect cells, such as primary T-cells and HSCs [30]. | Ex vivo engineering of CAR-T cells or editing HSCs for sickle cell disease. |
| CRISPR Screening Libraries | Pooled collections of gRNAs enabling genome-wide or pathway-focused functional genetic screens. | Identifying genes essential for cancer cell survival or therapy resistance. |
| Off-Target Prediction Software | In silico tools (often AI-powered) to predict potential off-target sites for a given gRNA [7]. | Pre-clinical safety assessment of gRNA candidates. |
| Base & Prime Editors | Next-generation editors that enable precise nucleotide changes or small insertions/deletions without inducing double-strand breaks [4] [7]. | Correcting a point mutation in the beta-globin gene for sickle cell disease. |
| Anti-MRSA agent 15 | Anti-MRSA agent 15, MF:C28H20F2N2O3, MW:470.5 g/mol | Chemical Reagent |
| HIV-1 inhibitor-79 | HIV-1 inhibitor-79, MF:C21H17N7O, MW:383.4 g/mol | Chemical Reagent |
The integration of CRISPR-Cas systems into therapeutic cell design has progressed from a revolutionary research concept to a validated clinical approach. The landscape in 2025 is characterized by the first approved CRISPR-based medicines, an expanding portfolio of clinical trials across diverse disease areas, and continued innovation in editing precision and delivery technologies. This application note provides a detailed overview of the current clinical landscape, summarizing approved therapies and active trial status, with specific protocols to support research and development activities in this rapidly advancing field.
Approved CRISPR-Based Therapies
As of 2025, the landmark approved CRISPR-based therapy is CASGEVY (exagamglogene autotemcel or exa-cel), which received regulatory approval in multiple regions beginning in late 2023 [8] [31] [32]. This therapy represents the first clinical validation of the CRISPR-Cas9 platform for human therapeutics.
Table 1: Approved CRISPR-Based Therapies (2025)
| Therapy Name | Indications | Target Gene | Editing Approach | Delivery Method | Approval Regions |
|---|---|---|---|---|---|
| CASGEVY (exa-cel) | Sickle cell disease (SCD), Transfusion-dependent beta thalassemia (TDT) | BCL11A | CRISPR-Cas9 knockout | ex vivo (CD34+ hematopoietic stem cells) | U.S., Great Britain, EU, Canada, Switzerland, Saudi Arabia, Bahrain, Qatar, UAE [32] |
| Commercial Status | Patient Access | Manufacturing | Clinical Outcomes | Treatment Process | Eligible Population |
| Commercial launch ongoing | ~300 patients referred, ~165 cell collections, 39 infusions as of September 2025 [32] | Non-viral, ex vivo editing | Elimination of vaso-occlusive crises (SCD) and transfusion requirements (TDT) [32] | Autologous cell transplant requiring myeloablative conditioning | >60,000 eligible patients across approved markets [32] |
Active Clinical Trials Landscape
The clinical development pipeline for CRISPR-based therapies has expanded significantly, with approximately 250 clinical trials involving gene-editing therapeutic candidates tracked as of February 2025, more than 150 of which are currently active [33]. These span multiple therapeutic areas and employ increasingly diverse editing platforms.
Table 2: Active Clinical Trials by Therapeutic Area (February 2025)
| Therapeutic Area | Number of Trials (Approx.) | Lead Candidates | Development Phase | Key Targets |
|---|---|---|---|---|
| Haematological Malignancies | 50+ | CTX112, CTX131 [32] | Phase I-III | CD19, CD70, B-cell maturation antigen |
| Cardiovascular Diseases | 10+ | VERVE-101, VERVE-102, VERVE-201, CTX310, CTX320 [33] [6] [34] | Phase I-II | PCSK9, ANGPTL3, LPA, AGT |
| Rare Genetic Diseases | 30+ | NTLA-2001, NTLA-2002, PM359 [8] [6] | Phase I-III | TTR (transthyretin), KLKB1, NCF1 |
| Autoimmune Diseases | 10+ | CTX112 [33] [32] | Phase I-II | CD19 (for SLE, systemic sclerosis) |
| Bacterial Diseases | 5+ | CRISPR-enhanced phage therapies [8] | Phase I-II | E. coli, urinary tract infections |
| Regenerative Medicine | 5+ | CTX211 (VCTX210A) [6] | Phase I/II | Stem cell-derived beta cells for Type 1 diabetes |
Promising Late-Stage Clinical Candidates
Several investigational therapies have advanced to late-stage clinical development, representing diverse therapeutic applications and technological approaches:
- NTLA-2001 (nexiguran ziclumeran): An in vivo CRISPR-Cas9 therapy targeting transthyretin amyloidosis (ATTR) currently in Phase III trials (NCT06128629). The therapy aims to reduce circulating TTR protein levels through single-dose knockout of the TTR gene [8] [6].
- NTLA-2002: A Phase III candidate for hereditary angioedema (HAE) that disables the KLKB1 gene via LNP-delivered CRISPR-Cas9, demonstrating 86% reduction in kallikrein and significant reduction in attacks in Phase I/II trials [8] [31] [6].
- CTX112: An allogeneic CAR-T cell therapy targeting CD19 with Regenerative Medicine Advanced Therapy (RMAT) designation, currently in Phase I trials for autoimmune diseases (SLE, systemic sclerosis, inflammatory myositis) and B-cell malignancies [32].
Experimental Protocols for CRISPR Therapeutic Development
Protocol: Ex Vivo Engineering of Hematopoietic Stem Cells (HSCs)
This protocol outlines the manufacturing process for autologous HSC therapies like CASGEVY [32] [4].
Materials and Reagents
- CD34+ hematopoietic stem cells from mobilized peripheral blood
- CRISPR-Cas9 ribonucleoprotein (RNP) complex
- Electroporation system
- Stem cell culture media with cytokines
- Myeloablative conditioning agent (e.g., busulfan)
Procedure
- Cell Collection and Isolation: Collect autologous CD34+ HSCs via apheresis following stem cell mobilization. Isulate CD34+ cells using clinical-grade magnetic-activated cell sorting.
- CRISPR RNP Complex Formation: Form ribonucleoprotein complexes by combining purified Cas9 protein with synthetic sgRNA targeting the therapeutic locus.
- Electroporation: Introduce RNP complexes into CD34+ cells via electroporation.
- Cell Expansion: Culture edited cells in cytokine-supplemented medium.
- Quality Control: Assess editing efficiency, cell viability, and sterility.
- Patient Conditioning: Administer myeloablative conditioning.
- Product Infusion: Transplant edited cells back to the patient.
Protocol: In Vivo Liver-Directed Editing via LNP Delivery
This protocol describes the approach for systemic administration of LNP-formulated CRISPR therapies [8] [34].
Materials and Reagents
- CRISPR mRNA and sgRNA
- Ionizable lipid nanoparticles
- Phosphate-buffered saline
- Sterile filtration system
Procedure
- Formulation Preparation: Encapsulate CRISPR-Cas9 mRNA and sgRNA in biodegradable LNPs.
- Quality Control: Assess particle size, encapsulation efficiency, and sterility.
- Dose Preparation: Dilute LNP formulation to appropriate concentration.
- Administration: Administer via intravenous infusion.
- Monitoring: Assess protein reduction and potential immune responses.
Key Technological Advances and Research Reagents
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for CRISPR Therapeutic Development
| Reagent Category | Specific Examples | Research Application | Clinical Relevance |
|---|---|---|---|
| Editing Platforms | CRISPR-Cas9, Cas12, Base editors, Prime editors | Target validation, efficacy studies | Clinical candidates using multiple platforms [33] [4] |
| Delivery Systems | LNPs, AAVs, Electroporation systems | In vivo and ex vivo delivery optimization | LNPs dominate liver-directed therapies [8] [31] |
| Cell Culture Systems | Cytokine cocktails, Serum-free media | Stem cell maintenance and differentiation | Critical for ex vivo manufacturing [32] |
| Analytical Tools | NGS for off-target analysis, Digital PCR | Safety and efficacy assessment | Regulatory requirement for clinical development [4] |
| Ethyl acetoacetate-d5 | Ethyl acetoacetate-d5, MF:C6H10O3, MW:135.17 g/mol | Chemical Reagent | Bench Chemicals |
| BAY-43-9695 | BAY-43-9695, CAS:233255-39-5, MF:C22H25N3O4S, MW:427.5 g/mol | Chemical Reagent | Bench Chemicals |
Visualization: CRISPR Therapeutic Development Workflow
The clinical landscape for CRISPR-based therapies in 2025 demonstrates robust growth with an approved product, CASGEVY, establishing clinical validation and multiple advanced candidates approaching commercialization. The field continues to evolve with improvements in delivery systems, editing precision, and manufacturing processes. Researchers and drug development professionals should monitor the progressing late-stage trials and incorporate the latest technological advances, particularly in LNP delivery and next-generation editing systems, to advance new therapeutic candidates.
Therapeutic Implementation: Ex Vivo and In Vivo Editing Strategies for Disease Treatment
Ex vivo cell engineering represents a paradigm shift in therapeutic development, wherein a patient's own cells are extracted, genetically modified outside the body, and then reinfused to treat disease [35]. This approach is particularly impactful in two key areas: the engineering of hematopoietic stem cells (HSCs) to cure genetic blood disorders and the development of chimeric antigen receptor (CAR) T-cells to combat cancer. The advent of CRISPR-Cas genome editing technology has dramatically accelerated both fields by enabling precise, targeted genetic modifications [36] [37].
CRISPR-Cas systems provide an unprecedented ability to rewrite genomic sequences, allowing researchers to correct disease-causing mutations in HSCs or enhance the tumor-fighting capabilities of T-cells [38]. Unlike in vivo editing, which poses delivery and safety challenges, ex vivo manipulation offers greater control over editing efficiency and specificity while facilitating comprehensive quality assessment before therapeutic application [35]. This document details the current protocols and applications of ex vivo genome editing across these two transformative therapeutic domains.
CRISPR-Cas Systems for Ex Vivo Editing
The CRISPR-Cas toolkit has expanded considerably beyond the original Cas9 nuclease, offering researchers multiple platforms suited to different therapeutic objectives. The table below compares the key CRISPR systems used in ex vivo cell engineering.
Table 1: Comparison of CRISPR Systems for Ex Vivo Cell Engineering
| System | Editing Action | Key Features | Primary Applications | Notable Advantages |
|---|---|---|---|---|
| CRISPR-Cas9 [36] [39] | DNA double-strand break (DSB) | NGG PAM requirement; creates blunt-end DSBs | Gene knockout (via NHEJ), gene insertion (via HDR) | High efficiency; well-characterized; versatile |
| CRISPR-Cas12a [39] [40] | DNA double-strand break (DSB) | TTTV PAM requirement; creates sticky-end DSBs | Gene knockout, gene insertion | Lower off-target rates; efficient multi-gene editing |
| Base Editors [37] [41] | Single-base conversion without DSB | A•T to G•C or C•G to T•A transitions | Point mutation correction | Avoids DSB-associated risks; high precision |
| Prime Editors [42] | Reverse transcription of new sequence | Does not require DSB or donor template | All 12 possible base-to-base changes, small insertions/deletions | Most versatile for point mutations; minimal byproducts |
| CRISPRa/i [40] | Gene expression modulation | dCas9 fused to activators/repressors | Transient gene activation or suppression | Reversible effect; no permanent genomic change |
The delivery format of CRISPR components significantly impacts editing efficiency and safety. For clinical applications, ribonucleoprotein (RNP) complexes (comprising purified Cas protein and synthetic guide RNA) are often preferred for transient activity that reduces off-target effects [36]. Alternatively, mRNA encoding Cas enzymes combined with synthetic guide RNAs offers a versatile balance between efficiency and transient exposure [41]. The choice between HDR and NHEJ pathways depends on the therapeutic goal: NHEJ is exploited for gene disruption, while HDR facilitates precise gene correction or insertion using donor templates [36] [43].
Application Note 1: Engineering of Hematopoietic Stem Cells (HSCs)
Therapeutic Rationale and Targets
Ex vivo editing of HSCs offers a curative potential for monogenic hematological disorders by enabling permanent correction of the causative mutation within the entire hematopoietic system [43]. Edited HSCs can engraft in the bone marrow and continuously produce healthy, genetically corrected blood cells throughout a patient's lifetime. Prime examples include sickle cell disease (SCD) and β-thalassemia, both caused by mutations in the β-globin gene (HBB) [42].
Two primary strategic approaches have emerged:
- Direct Correction: Technologies like prime editing can directly revert the pathogenic E6V mutation in the HBB gene back to the wild-type sequence, representing the most physiological correction [42].
- Indirect Therapeutic Strategies: Nuclease-based approaches can disrupt regulatory genes such as BCL11A, a natural repressor of fetal hemoglobin (HbF). This disruption reactivates HbF production, which compensates for the defective adult hemoglobin and ameliorates disease symptoms [44].
Critical Protocol: Ex Vivo Culture for High-Efficiency HSC Editing
A major challenge in HSC editing is balancing high editing efficiency with the preservation of stem cell "stemness" — their long-term self-renewal and multi-lineage repopulation capacity. Prolonged ex vivo culture and stimulation can detrimentally impact HSC engraftment potential [43]. The protocol below, optimized by Rai et al., addresses this challenge through fine-tuned culture conditions [43].
Table 2: Optimized Culture Media Composition for HSC Editing [43]
| Component | Function | Basal Medium | IL-3 Based | Stemness-Preserving (IL-6 Based) |
|---|---|---|---|---|
| FLT3L, TPO, SCF | Essential stem cell agonists | ✓ | ✓ | ✓ |
| IL-3 | Promotes proliferation and HDR | ✗ | 20-60 ng/mL | ✗ |
| IL-6 | Better preservation of stemness | ✗ | ✗ | ✓ |
| SR-1, UM171 | Small molecule stemness agonists | ✗ | ✗ | ✓ |
| HDAC Inhibitors | May improve chromatin access for editing | ✗ | Under investigation | Under investigation |
Workflow Overview:
- HSPC Isolation: Isolate CD34+ HSPCs from mobilized peripheral blood or bone marrow.
- Pre-stimulation: Culture cells for 2 days in a serum-free medium supplemented with FLT3L, TPO, SCF, and a cytokine composition chosen based on the strategic priority (e.g., IL-3 for higher HDR efficiency vs. IL-6 for superior stemness preservation) [43].
- Gene Editing: Deliver CRISPR components (e.g., Cas9 RNP) alongside the AAV6 donor template via electroporation and transduction [43].
- Post-editing Culture: Maintain cells for 2-4 more days in the optimized medium to allow for editing and recovery.
- Transplantation: Infuse the edited HSPCs back into the patient after conditioning.
Key Outcomes: Using this optimized protocol, researchers achieved HDR-mediated knock-in efficiencies of up to 42% in IL-3 supplemented media, significantly higher than the 27% observed with stemness-preserving conditions. This protocol successfully balances the critical trade-off between high editing efficiency and the preservation of long-term repopulating HSCs, which is essential for durable therapeutic effects [43].
The following diagram illustrates the logical decision-making process for optimizing HSC editing protocols, balancing the critical trade-off between high editing efficiency and the preservation of long-term repopulating capacity.
Application Note 2: Engineering of CAR-T Cells
Therapeutic Rationale and Targets
CAR-T cell therapy has demonstrated remarkable success, particularly against B-cell malignancies. However, challenges remain, including limited efficacy in solid tumors, product toxicity, T-cell exhaustion, and the costly, time-consuming autologous manufacturing process [36] [40]. CRISPR-based engineering is being deployed to overcome these hurdles through precise genomic modifications.
Key engineering strategies include:
- Enhancing Potency and Persistence: Knocking out negative immune regulators (e.g., PDCD1 [PD-1], TIGIT) to prevent T-cell exhaustion [39] [40].
- Improving Safety: Knocking out the endogenous TCRα constant chain (TRAC) to prevent graft-versus-host disease (GvHD) in allogeneic "off-the-shelf" products, and eliminating genes like FAS to reduce activation-induced cell death [41].
- Enabling Universal Products: Disrupting the TRAC and B2M loci to generate allogeneic CAR-T cells that are less likely to be rejected by the host immune system [40].
- Preventing Fratricide: Modifying surface antigens to prevent CAR-T cells from attacking each other during manufacturing [41].
Advanced Protocol: Multi-Gene Editing for Next-Generation CAR-T Cells
This protocol describes the generation of allogeneic, multi-gene edited CAR-T cells using the CRISPR-Cas12a system, which is particularly suited for complex engineering due to its high specificity and efficiency in multiplexed knock-in [39] [40].
Workflow Overview:
- T-cell Activation: Isolate primary human T-cells and activate them using anti-CD3/CD28 antibodies.
- CRISPR Component Delivery: Electroporate T-cells with Cas12a RNP complexes. Cas12a Ultra, a high-efficacy variant, is recommended for superior knockout and knockin efficiency, achieving single transgene knockin in up to 60% of T-cells [39].
- CAR Gene Integration: Simultaneously transduce cells with an AAV6 vector carrying the CAR transgene flanked by homology arms, targeting its insertion into a specific genomic safe harbor (e.g., TRAC locus) via HDR. The Cas12a system has demonstrated a seven-fold increase in simultaneous knockin efficiency compared to Cas9 in some studies [39].
- Expansion and Validation: Expand the edited T-cells and validate editing efficiency (via NGS), CAR expression (via flow cytometry), and function (via cytotoxicity assays).
Key Discoveries from High-Throughput Screening: The CELLFIE platform, a CRISPR screening tool, has enabled the unbiased discovery of novel gene targets that enhance CAR-T cell function. Genome-wide knockout screens in primary human CAR-T cells identified RHOG and FAS as potent enhancers of anti-tumor efficacy [41]. RHOG knockout was a particularly unexpected discovery, as its deficiency causes immunodeficiency in humans, highlighting how evolutionary constraints on natural T-cells differ from the requirements for short-term therapeutic CAR-T cell efficacy. The double knockout of RHOG-and-FAS showed synergistic effects, strongly enhancing anti-tumor activity in vivo [41].
The workflow below details the specific steps involved in the CELLFIE screening platform and the subsequent production of enhanced CAR-T cells based on the discovered genetic targets.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Ex Vivo Cell Engineering Protocols
| Reagent / Tool | Function | Example Use Case | Key Considerations |
|---|---|---|---|
| High-Fidelity Cas9 RNP [36] [43] | Complex of purified Cas9 protein and synthetic gRNA for high-efficiency, transient editing. | Knocking out PD-1 or TRAC in CAR-T cells. | Reduces off-target effects compared to plasmid delivery. |
| AAV6 Donor Vector [43] [42] | High-efficiency delivery of HDR template for precise gene insertion or correction. | Inserting a CAR gene into the TRAC locus or correcting the HBB gene in HSCs. | High transduction efficiency in HSCs and T-cells; limited packaging capacity. |
| PEmax mRNA [42] | An optimized prime editor architecture delivered as mRNA for DSB-free editing. | Correcting the SCD point mutation in HBB without creating DSBs. | Requires co-delivery of epegRNA and nicking sgRNA. |
| Cytokine Cocktails (FLT3L, TPO, SCF) [43] | Essential for ex vivo survival, proliferation, and maintenance of HSPCs. | Pre-stimulation of CD34+ HSPCs prior to gene editing. | IL-3 boosts HDR but may promote differentiation; IL-6 better preserves stemness. |
| Stemness Agonists (SR-1, UM171) [43] | Small molecules that help maintain the long-term repopulating capacity of HSCs during culture. | Added to HSPC culture medium to counteract the negative effects of prolonged ex vivo culture. | Critical for ensuring durable engraftment of edited HSCs. |
| CROP-seq-CAR Vector [41] | An integrated screening vector that co-delivers a CAR and a gRNA for pooled CRISPR screens. | Enabling genome-wide CRISPR screens in primary CAR-T cells to discover enhancer genes. | Links gRNA identity to phenotypic readout in individual cells. |
| BAY38-7690 | BAY38-7690, MF:C19H16ClF2N3O2, MW:391.8 g/mol | Chemical Reagent | Bench Chemicals |
| Atazanavir-d9 | Atazanavir-d9, MF:C38H52N6O7, MW:704.9 g/mol | Chemical Reagent | Bench Chemicals |
Safety and Analytical Considerations
The therapeutic application of CRISPR-edited cells necessitates rigorous safety assessment. Beyond the well-known concern of off-target editing, recent studies reveal a more pressing challenge: on-target structural variations (SVs) [44]. These include large deletions (kilobase- to megabase-scale), chromosomal rearrangements, and translocations that can be missed by standard short-read amplicon sequencing.
Critical Recommendations:
- Comprehensive Analysis: Employ genome-wide, unbiased methods like CAST-Seq or LAM-HTGTS to detect SVs and translocations that traditional sequencing might overlook [44].
- Caution with HDR Enhancers: The use of DNA-PKcs inhibitors (e.g., AZD7648) to boost HDR rates can dramatically increase the frequency of these large genomic aberrations, both on-target and off-target. Their application requires careful risk-benefit analysis [44].
- Safety-by-Design: Whenever possible, opt for editing strategies that avoid double-strand breaks, such as base editing or prime editing, which are associated with significantly lower rates of genotoxic side effects [42].
Ex vivo engineering of HSCs and T-cells using CRISPR technologies has moved from concept to clinical reality. Optimized protocols for HSC culture and the development of advanced CRISPR tools like Cas12a and prime editors are enabling the creation of more effective and safer therapeutic products. The integration of high-throughput screening platforms such as CELLFIE is systematically uncovering novel genetic modifications that enhance cell function beyond naturally evolved capabilities. As the field progresses, a steadfast commitment to comprehensive genomic safety profiling will be paramount to realizing the full therapeutic potential of these groundbreaking engineered cell therapies.
The therapeutic application of CRISPR-Cas genome editing represents a paradigm shift in therapeutic cell design research, offering potential cures for genetic disorders, cancers, and infectious diseases. The efficacy of these groundbreaking therapies is fundamentally constrained by the delivery vectors that transport CRISPR components to target cells in vivo. The two primary delivery platforms—viral vectors and lipid nanoparticles (LNPs)—each present distinct advantages and limitations that researchers must carefully balance for specific therapeutic applications. Viral vectors, particularly adeno-associated viruses (AAVs), have historically dominated clinical gene therapy due to their high transduction efficiency, while LNPs have emerged as a versatile non-viral alternative with superior safety profiles and manufacturing advantages. This application note provides a detailed comparative analysis of these platforms, supported by quantitative data, standardized protocols, and visual workflows to guide researchers in selecting and implementing optimal delivery strategies for CRISPR-based therapeutics.
Comparative Analysis of Delivery Platforms
Fundamental Mechanisms and Characteristics
Viral Vectors utilize the innate infectious mechanisms of genetically engineered viruses to deliver genetic material. AAVs, the most commonly used viral vector for CRISPR delivery, enter cells via receptor-mediated endocytosis, escape the endosome, and translocate to the nucleus where the single-stranded DNA genome is released. The delivered transgene, which typically encodes the Cas9 nuclease and guide RNA (gRNA), leverages the host cell's transcriptional machinery to express the editing components over an extended period. Lentiviral vectors (LVs) offer the additional capability of integrating into the host genome, enabling permanent gene modification, though this introduces risks of insertional mutagenesis [45] [46].
Lipid Nanoparticles are synthetic, multi-component vesicles typically measuring 50-120 nm in diameter that encapsulate nucleic acid payloads through self-assembly. LNPs predominantly enter cells via endocytosis following systemic administration. The key functional component—ionizable cationic lipids—undergoes protonation in the acidic endosomal environment, facilitating fusion with the endosomal membrane and subsequent release of the nucleic acid payload into the cytoplasm. For CRISPR applications, LNPs can deliver various cargo formats including mRNA encoding Cas9 combined with gRNA, or preassembled ribonucleoprotein (RNP) complexes of Cas9 protein and gRNA [47] [48].
Table 1: Core Components and Functional Roles of Lipid Nanoparticles
| Component | Concentration Range | Primary Function | Considerations |
|---|---|---|---|
| Ionizable Cationic Lipid | 30-60 mol% | Encapsulates nucleic acids; facilitates endosomal escape via pH-dependent protonation | Critical for efficiency; optimization reduces toxicity |
| Phospholipid | 5-20 mol% | Stabilizes LNP structure; influences bilayer properties | Enhances particle stability and fusion capacity |
| Cholesterol | 25-40 mol% | Modulates membrane fluidity and integrity | Improves circulation half-life and cellular uptake |
| PEG-Lipid | 1-5 mol% | Shields surface charge; reduces clearance; controls particle size | Higher percentages can inhibit cellular uptake |
Quantitative Comparison of Performance Metrics
The selection between viral vectors and LNPs requires careful consideration of multiple performance parameters. The following table synthesizes comparative data from recent preclinical and clinical studies to inform platform selection.
Table 2: Performance Comparison of Viral Vectors vs. LNPs for CRISPR Delivery
| Parameter | Viral Vectors (AAV) | Lipid Nanoparticles (LNP) | Key Implications |
|---|---|---|---|
| Payload Capacity | Limited (~4.7 kb) often requiring dual vectors | Higher capacity (>10 kb); flexible cargo formats | LNP accommodates larger editors and complex constructs |
| Editing Duration | Long-term/stable (weeks-months) | Transient (days-week) | LNP reduces off-target risks; AAV suitable for permanent correction |
| Immunogenicity | High; pre-existing immunity common | Lower; suitable for redosing | LNP enables multiple administrations; AAV limited to single dose |
| Manufacturing Timeline | Complex; several weeks | Streamlined; 1-2 days | LNP offers rapid production advantage |
| Liver Editing Efficiency | Moderate to high (varies by serotype) | High (16-37% with iGeoCas9 RNP-LNPs) [49] | Both effective for hepatic targets |
| Lung Editing Efficiency | Variable | 16-19% with optimized RNP-LNPs [49] | LNP demonstrates superior non-liver tissue editing |
| Tissue Targeting Precision | Excellent with engineered capsids | Primarily liver-tropic; targeting ligands under development | AAV superior for extrahepatic tissues without modification |
Experimental Protocols and Methodologies
LNP Formulation for CRISPR RNP Delivery
This protocol details the formulation of LNPs encapsulating CRISPR ribonucleoprotein complexes based on the recently published methodology that achieved 19% editing efficiency in lung tissue [49].
Materials and Reagents
- Ionizable Lipid: ALC-0315 or biodegradable equivalent (e.g., ALC-0307)
- Helper Lipids: DSPC (1,2-distearoyl-sn-glycero-3-phosphocholine), cholesterol
- PEG-Lipid: ALC-0159 or equivalent DMG-PEG
- Cas9 RNP Complex: iGeoCas9 variant complexed with target-specific sgRNA
- Microfluidic Device: NanoAssemblr, Precision NanoSystems NxGen
- Formulation Buffer: 10 mM citrate, pH 4.0
- Dialysis Equipment: 10K MWCO membranes, PBS buffer
Procedure
- Lipid Solution Preparation: Prepare lipid mixture in ethanol containing ionizable lipid (50 mol%), DSPC (10 mol%), cholesterol (38.5 mol%), and PEG-lipid (1.5 mol%). Maintain total lipid concentration at 10-12 mM.
Aqueous Phase Preparation: Dilute Cas9 RNP complexes (preassembled at 3:1 molar ratio of Cas9:sgRNA) in citrate formulation buffer to final concentration of 100 μg/mL.
Microfluidic Mixing: Utilize staggered herringbone micromixer with aqueous:organic flow rate ratio of 3:1. Set total flow rate at 12 mL/min to achieve rapid mixing.
Buffer Exchange and Dialysis: Immediately dilute formulated LNPs in 1X PBS (pH 7.4) at 1:5 ratio. Dialyze against 1000X volume PBS for 4 hours at 4°C with one buffer change after 2 hours.
Concentration and Sterilization: Concentrate using 100K MWCO centrifugal filters to desired concentration (typically 1-2 mg/mL lipid). Sterilize through 0.22 μm PES membrane filter.
Quality Assessment: Determine particle size (target: 80-100 nm), PDI (<0.2), encapsulation efficiency (>90%) via RiboGreen assay, and editing potency in vitro.
In Vivo Evaluation of CRISPR-LNP Formulations
Animal Model Considerations
- Utilize Ai9 tdTomato reporter mice for quantitative editing assessment
- For disease models: select appropriate models (e.g., hereditary transthyretin amyloidosis for liver editing, SFTPC mutations for lung editing)
Dosing Protocol
- Administration Route: Intravenous injection via tail vein
- Dosage: 1-3 mg lipid/kg body weight for RNP-LNPs; 0.5-1 mg/kg for mRNA-LNPs
- Dosing Schedule: Single administration for efficacy; multiple doses (2-4 week intervals) for redosing studies
- Control Groups: Include empty LNP, non-targeting gRNA, and vehicle controls
Tissue Collection and Analysis
- Necropsy Timing: 7-14 days post-administration for peak editing assessment
- Tissue Processing: Homogenize entire liver/left lung for bulk analysis; preserve right lung for histology
- Editing Quantification:
- Next-generation sequencing of PCR-amplified target loci
- T7 Endonuclease I assay for initial screening
- Immunohistochemistry for functional protein expression
- Plasma protein levels (e.g., TTR reduction for hATTR models)
Research Reagent Solutions
Table 3: Essential Reagents for CRISPR Delivery Research
| Reagent Category | Specific Examples | Research Application | Supplier Considerations |
|---|---|---|---|
| Ionizable Lipids | ALC-0315, DLin-MC3-DMA, SM-102 | LNP self-assembly and endosomal escape | Commercial availability vs. proprietary synthesis |
| Cas9 Enzymes | SpyCas9, GeoCas9, iGeoCas9 variants | Genome editing catalysis | Thermostability, PAM requirements, licensing |
| Guide RNA | Chemically modified sgRNA, truGuide | Target sequence recognition | GMP-grade for clinical translation; chemical modifications for stability |
| Microfluidic Devices | NanoAssemblr, NxGen | Reproducible LNP formation | Throughput capacity, scalability, cost |
| AAV Serotypes | AAV2, AAV8, AAV9, AAVrh.10 | Tissue-specific tropism | Packaging capacity, immunogenicity profile, production yield |
| Analytical Standards | NISTmAb, lipoprotein standards | LNP characterization and quality control | Regulatory compliance, assay standardization |
Visual Workflows and Signaling Pathways
LNP-Mediated CRISPR Delivery Mechanism
Diagram 1: Intracellular trafficking pathway of LNP-CRISPR delivery, highlighting endosomal escape as the critical rate-limiting step.
Platform Selection Algorithm
Diagram 2: Decision algorithm for selecting between viral vector and LNP delivery platforms based on therapeutic requirements.
Emerging Applications and Future Directions
The application landscape for CRISPR delivery platforms is rapidly expanding beyond monogenic diseases. Recent clinical advances demonstrate the remarkable potential of both viral and non-viral delivery systems. In 2025, a landmark study reported the first personalized in vivo CRISPR therapy for an infant with carbamoyl-phosphate synthetase 1 (CPS1) deficiency delivered via LNP. The therapy was developed and administered within six months, with the patient safely receiving three escalating doses that demonstrated improved symptoms with each administration [8]. This case establishes a new paradigm for rapid-response, bespoke genomic medicines.
Concurrently, Intellia Therapeutics has demonstrated the redosing capability of LNP-based CRISPR therapeutics in their Phase I trial for hereditary transthyretin amyloidosis (hATTR), where participants receiving the higher dose showed approximately 90% reduction in disease-related TTR protein levels sustained over two years [8]. These clinical successes highlight the transformative potential of LNP delivery for CRISPR therapeutics.
Future development priorities include expanding tissue tropism beyond hepatic focus through surface functionalization with targeting ligands such as Designed Ankyrin Repeat Proteins (DARPins), which have demonstrated up to 98% binding and 90% expression in human CD8+ T cells [48]. The emergence of thermostable Cas9 variants like iGeoCas9, which enable efficient RNP delivery to lung tissue with 19% editing efficiency in the disease-causing SFTPC gene, represents another significant advancement [49]. As the field progresses, establishing standardized safety profiles for repeated LNP administration and developing scalable manufacturing processes will be critical for broadening patient access to these revolutionary therapies.
The advent of CRISPR-Cas genome editing has ushered in a transformative era for therapeutic cell design, enabling precise genomic modifications previously unattainable. This application note details the clinical protocols and outcomes for two landmark CRISPR-based therapies: Casgevy (exagamglogene autotemcel) for sickle cell disease (SCD) and investigational CRISPR therapies for hereditary transthyretin amyloidosis (hATTR). These cases exemplify the dual therapeutic paradigms of ex vivo and in vivo genome editing, providing a framework for researchers and drug development professionals engaged in translating gene editing technologies into clinical practice. The data presented herein, including recent 2025 clinical updates, highlight both the remarkable efficacy and the persisting challenges within the CRISPR therapeutic landscape [8].
Clinical Outcomes and Quantitative Data Analysis
The efficacy of these therapies is demonstrated through rigorous clinical trials. The quantitative outcomes from these studies are summarized in the tables below to facilitate direct comparison of key efficacy and safety endpoints.
Table 1: Primary Efficacy Endpoints from Pivotal Clinical Trials
| Therapeutic Agent | Disease | Trial Phase & Design | Primary Efficacy Endpoint Result |
|---|---|---|---|
| Casgevy [50] | Sickle Cell Disease (SCD) | Open-label, single-arm trial (N=44 treated, N=31 evaluated for efficacy) | 29 of 31 (93.5%) participants were free of severe vaso-occlusive crises (VOCs) for at least 12 consecutive months post-treatment. |
| Intellia's CRISPR Therapy [8] | Hereditary ATTR (hATTR) with Polyneuropathy | Phase I trial (N=27 at 2-year follow-up) | Sustained mean reduction of ~90% in serum TTR protein levels at 2 years post-treatment. |
| Intellia's CRISPR Therapy [8] | Hereditary Angioedema (HAE) | Phase I/II trial (N=11 in high-dose cohort) | 86% average reduction in plasma kallikrein levels; 8 of 11 (73%) participants were attack-free during the 16-week observation period post-treatment. |
Table 2: Key Safety and Tolerability Profile from Clinical Trials
| Therapeutic Agent | Most Common Side Effects | Serious Risks & Management |
|---|---|---|
| Casgevy [50] | Low levels of platelets and white blood cells (due to conditioning regimen). | Requires prolonged hospitalization (∼4-6 weeks) for monitoring and management of cytopenias until engraftment. Rescue cell infusion is available if manufacturing or engraftment fails. |
| Intellia's CRISPR Therapy (LNP-delivered) [8] | Mild to moderate infusion-related reactions. | Favorable safety profile observed; no serious side effects reported in the hATTR and HAE trials. The LNP delivery system enables the possibility of re-dosing, as demonstrated in clinical practice. |
Experimental Protocols and Workflows
Protocol 1: Ex Vivo Manufacturing of Casgevy for Sickle Cell Disease
The production of Casgevy is an ex vivo process where patient-derived cells are genetically modified outside the body.
Step 1: Hematopoietic Stem and Progenitor Cell (HSPC) Mobilization and Apheresis
- Patients receive a mobilization agent (e.g., plerixafor) to mobilize HSPCs from the bone marrow into the peripheral blood.
- HSPCs are collected via leukapheresis. This process may be repeated to obtain a sufficient cell dose.
- A portion of the collected cells is cryopreserved as unmodified "rescue cells" to be used in case of treatment failure [50].
Step 2: CRISPR-Cas9 Genome Editing
- The CD34+ HSPCs are isolated and electroporated with CRISPR-Cas9 components.
- The guide RNA (gRNA) is designed to target the BCL11A gene enhancer region.
- The Cas9 nuclease induces a double-strand break at the target site.
- The break is repaired via non-homologous end joining (NHEJ), resulting in gene disruption [38].
Step 3: Patient Conditioning and Reinfusion
- Patients undergo myeloablative conditioning with busulfan to clear the bone marrow niche for the edited cells.
- The CRISPR-edited CD34+ cells (the final drug product, Casgevy) are thawed and administered via intravenous infusion.
- Patients are hospitalized for approximately 4-6 weeks for supportive care until neutrophil and platelet engraftment is confirmed [50].
The following workflow diagram illustrates this multi-stage process:
Protocol 2: In Vivo CRISPR Therapy for hATTR
The therapy for hATTR represents a streamlined in vivo approach, where the editing components are administered directly to the patient.
Step 1: Formulation of CRISPR-LNP
Step 2: Clinical Dosing and Monitoring
- The LNP formulation is administered as a single intravenous infusion. Clinical trials have explored multiple dosing levels.
- Notably, the use of LNPs avoids the immunogenic risks associated with viral vectors, allowing for the possibility of re-dosing, which has been successfully implemented in clinical practice [8].
- Efficacy is monitored by measuring serum TTR protein levels as a pharmacodynamic biomarker.
- Disease progression is assessed using standardized measures such as the Neuropathy Impairment Score (NIS) and quality-of-life questionnaires [8] [52].
The following workflow diagram illustrates this direct in vivo administration process:
The Scientist's Toolkit: Research Reagent Solutions
The development and execution of these therapies rely on a suite of critical research reagents and platforms.
Table 3: Essential Research Reagents and Tools for CRISPR Therapeutic Development
| Reagent / Tool | Function in Therapy Development | Specific Example in Featured Therapies |
|---|---|---|
| Lipid Nanoparticles (LNPs) [8] [51] | In vivo delivery vehicle for CRISPR machinery; protects nucleic acids and facilitates cellular uptake. | Used for systemic delivery of Cas9 mRNA and gRNA to hepatocytes in hATTR and HAE therapies. |
| Guide RNA (gRNA) [38] | Provides targeting specificity by binding to Cas protein and complementary DNA sequence. | BCL11A enhancer-targeting gRNA (Casgevy); TTR gene-targeting gRNA (hATTR therapy). |
| Cas Nuclease [8] [38] | Effector protein that creates double-strand breaks in target DNA. | Cas9 nuclease is used in both Casgevy and the hATTR therapies. |
| Electroporation Systems | Enables ex vivo delivery of CRISPR components into hard-to-transfect cells (e.g., HSPCs). | Used to introduce CRISPR-Cas9 ribonucleoproteins into CD34+ cells during Casgevy manufacturing. |
| Single-Cell DNA Sequencing [53] | High-resolution analysis of editing outcomes (on-target efficiency, zygosity, structural variations). | Platforms like Tapestri characterize clonality and editing patterns in triple-edited cell products. |
| AI-Designed Editors [9] | Novel CRISPR effectors generated computationally with optimized properties (e.g., activity, size). | OpenCRISPR-1 is an AI-generated Cas9 variant with high activity and specificity for potential future therapeutics. |
| UCI-1 | UCI-1, MF:C33H45N7O7, MW:651.8 g/mol | Chemical Reagent |
| Janthinocin B | Janthinocin B, MF:C57H82N12O16, MW:1191.3 g/mol | Chemical Reagent |
The clinical success of Casgevy for SCD and the promising late-stage trials for hATTR therapies validate CRISPR-Cas9 as a powerful platform for therapeutic cell design. The contrasting methodologies—ex vivo engineering of HSPCs versus in vivo systemic administration—highlight the versatility of the technology. Key to this progress has been the evolution of delivery systems, particularly LNPs for in vivo delivery. Furthermore, the advent of AI-designed editors and advanced analytical tools like single-cell sequencing promises to enhance the safety, efficacy, and scope of the next generation of CRISPR-based medicines. Despite challenges in manufacturing, cost, and funding, these therapies represent a paradigm shift in treating genetic diseases at their molecular root [8] [9] [53].
The evolution of CRISPR-Cas systems has progressed beyond simple nuclease-based gene disruption to a suite of precision tools that enable unprecedented control over genomic information. While traditional CRISPR-Cas9 creates double-strand breaks (DSBs) that activate endogenous DNA repair pathways, this process can lead to unpredictable outcomes including indels and chromosomal rearrangements [54] [55]. Advanced editing platforms—base editing, prime editing, and epigenome modulation—have emerged to address these limitations, offering enhanced precision and expanded therapeutic potential for therapeutic cell design research.
These third-generation editing technologies minimize or eliminate DSB formation, thereby reducing unintended consequences while enabling more diverse genetic and epigenetic modifications. Base editing facilitates direct chemical conversion of one DNA base to another without DSBs, prime editing operates as a "search-and-replace" system for precise small edits, and epigenome editing allows reversible modulation of gene expression without altering the DNA sequence itself [55] [56] [57]. For researchers and drug development professionals engineering therapeutic cells, these platforms provide increasingly sophisticated tools to correct pathogenic mutations, regulate gene expression networks, and develop novel cell therapies with enhanced safety profiles.
Base Editing
Base editors represent a significant advancement beyond nuclease-dependent CRISPR systems by enabling direct chemical conversion of one DNA base pair to another without inducing DSBs. These systems utilize catalytically impaired Cas proteins fused to nucleotide deaminase enzymes that mediate targeted base transitions through chemical modification [55]. Cytosine base editors (CBEs) catalyze C•G to T•A conversions, while adenine base editors (ABEs) facilitate A•T to G•C changes. The editing window typically spans nucleotides 4-8 within the protospacer, with efficiency influenced by sequence context, editor architecture, and cellular delivery method.
Recent innovations have expanded base editing capabilities, including the development of Cas12f-based cytosine base editors that unexpectedly gained the ability to edit both target and non-target DNA strands. Through focused mutagenesis and optimization, researchers have developed strand-selectable miniature base editors, including TSminiCBE, which preferentially targets the target strand and has demonstrated successful in vivo base editing in mice [7]. This compact editor is particularly valuable for therapeutic applications due to its compatibility with viral delivery vectors. In comparative studies for sickle cell disease, base editing outperformed traditional CRISPR-Cas9 in reducing red cell sickling despite similar engraftment rates, demonstrating higher editing efficiency with fewer genotoxicity concerns [7].
Prime Editing
Prime editing represents a paradigm shift in precision genome engineering by functioning as a versatile "search-and-replace" system that can mediate all possible base-to-base conversions, small insertions, and deletions without requiring DSBs or donor DNA templates [55]. The system comprises a prime editor protein—a Cas9 nickase (H840A) fused to an engineered reverse transcriptase (RT)—programmed with a specialized prime editing guide RNA (pegRNA). The pegRNA both specifies the target site and encodes the desired edit via its reverse transcriptase template (RTT) sequence.
The molecular mechanism involves: (1) binding of the prime editor complex to the target DNA, (2) nicking of the non-target strand by the nickase Cas9, (3) extension of the 3'-OH group by RT using the RTT, and (4) resolution of the resulting DNA heteroduplex to incorporate the edit into the genome [55]. This sophisticated mechanism enables precise installation of targeted changes with minimal byproducts.
Prime editing systems have evolved through several generations with significant improvements in efficiency. While the initial PE1 system demonstrated proof-of-concept with ~10-20% editing efficiency in HEK293T cells, subsequent versions incorporated various optimizations [55]. PE2 featured an engineered RT with enhanced processivity, doubling editing efficiency to ~20-40%. PE3 introduced an additional sgRNA to nick the non-edited strand, further increasing efficiency to ~30-50%. More recent versions (PE4-PE7) incorporate mismatch repair inhibitors and pegRNA stabilizers, achieving efficiencies up to 80-95% in human cells [55].
The technology has demonstrated remarkable therapeutic potential, exemplified by a prime editing strategy correcting pathogenic COL17A1 variants causing junctional epidermolysis bullosa. Researchers achieved up to 60% editing efficiency in patient keratinocytes, successfully restoring functional type XVII collagen. In xenograft models, gene-corrected cells demonstrated a powerful selective advantage, expanding from 55.9% of input cells to populate 92.2% of the skin's basal layer within six weeks [7].
Epigenome Modulation
Epigenome editing represents a fundamentally different approach by enabling reversible modulation of gene expression without altering the underlying DNA sequence [56]. These systems utilize catalytically dead Cas proteins (dCas9) fused to epigenetic effector domains that can establish or remove DNA methylation and histone modifications. Unlike conventional CRISPR systems that permanently change DNA sequence, epigenome editors establish stable but potentially reversible gene expression states, making them particularly suitable for regulating genes involved in complex diseases and cell differentiation.
The CRISPRoff system exemplifies this technology, synthetically fusing dCas9 to DNMT3A-DNMT3L (DNMT3A-3L) for DNA methylation and the KRAB transcriptional repressor domain for recruiting repressive histone modifications [57]. This system enables programmable "hit-and-run" epigenetic silencing—transient editor expression establishes stable, heritable epigenetic marks that persist through cell divisions. A complementary TET1-dCas9 activator can reverse these changes by enzymatically removing repressive DNA methylation [57].
Recent advances have addressed delivery challenges through innovative platforms like RENDER (Robust ENveloped Delivery of Epigenome-editor Ribonucleoproteins), which enables transient delivery of CRISPR epigenome editor ribonucleoproteins into human cells [57]. This system leverages engineered virus-like particles (eVLPs) derived from retroviruses to deliver large epigenome editors as ribonucleoprotein complexes, combining the advantages of transient delivery with the durability of epigenetic modifications.
The therapeutic potential of epigenome modulation is substantial. Researchers have silenced Pcsk9 in mice using a single LNP-administered dose of mRNA-encoded epigenetic editors, reducing PCSK9 by ~83% and LDL-C by ~51% for six months [7]. Additionally, Japanese researchers have employed CRISPR-based epigenome editing to demethylate the Prader-Willi syndrome imprinting control region in patient-derived iPSCs, successfully reactivating silenced maternal genes [7].
Table 1: Comparative Analysis of Advanced Editing Platforms
| Feature | Base Editing | Prime Editing | Epigenome Modulation |
|---|---|---|---|
| Editing Type | Chemical base conversion | Targeted insertions, deletions, all base substitutions | DNA methylation, histone modifications |
| DSB Formation | No | No | No |
| Therapeutic Example | Sickle cell disease (reducing sickling) | Junctional epidermolysis bullosa (COL17A1 correction) | Prader-Willi syndrome (imprinting control) |
| Efficiency Range | Varies by system; base editing outperformed CRISPR-Cas9 in SCD models [7] | 10-95% (depending on PE version and cell type) [55] | Up to 83% protein reduction sustained for 6 months in mouse models [7] |
| Key Limitation | Restricted to specific base transitions; bystander edits | Complex pegRNA design; variable efficiency across loci | Potential for off-target epigenetic modifications |
| Delivery Considerations | Compatible with viral vectors; compact versions available | Large size challenges viral delivery; LNPs promising | RENDER platform enables RNP delivery [57] |
Experimental Protocols
Base Editing Protocol for Therapeutic Cell Engineering
This protocol details the application of base editing for installing therapeutic point mutations in primary human T-cells for adoptive cell therapy, incorporating the latest Cas12f-based miniature editors for enhanced delivery [7].
Materials Required:
- Base editor plasmid (e.g., TSminiCBE for compact size or ABE8e for high efficiency)
- Target-specific sgRNA (designed with optimal positioning within editing window)
- Primary human T-cells from donor apheresis
- Activation beads (anti-CD3/CD28)
- Delivery system (lentiviral vectors for stable expression or LNPs for transient delivery)
- Editing efficiency validation reagents (tracking indels by decomposition-TIDE, deep sequencing)
Step-by-Step Procedure:
sgRNA Design and Validation: Design sgRNAs with the target base positioned within the optimal editing window (typically positions 4-8 for SpCas9-based editors). For TSminiCBE, consider strand preference in design. Validate sgRNA efficiency using a GFP-reporter system before therapeutic application.
Editor Delivery: For viral delivery, produce high-titer lentivirus carrying the base editor and sgRNA. Transduce activated T-cells at an MOI of 10-50 in the presence of 8μg/mL polybrene via spinfection (1000×g, 90 minutes, 32°C). For LNP delivery, formulate editor mRNA and sgRNA into LNPs using a microfluidic mixer and treat cells at 0.5mg/mL mRNA concentration.
Cell Culture and Editing: Activate primary T-cells with anti-CD3/CD28 beads at 1:1 bead:cell ratio in X-VIVO 15 media with 5% human AB serum and 100IU/mL IL-2. Transduce cells 24 hours post-activation. Maintain cells at 0.5-2×10^6 cells/mL throughout the editing window.
Editing Validation: Harvest cells 72 hours post-editing. Extract genomic DNA and amplify target regions by PCR. Assess editing efficiency by next-generation sequencing (minimum 10,000x coverage) or, for rapid screening, use TIDE decomposition analysis (sensitivity >5%).
Functional Validation: For therapeutic applications, evaluate functional consequences of editing through: (1) Western blot for protein expression changes, (2) Flow cytometry for surface marker alterations, (3) In vitro functional assays (e.g., cytokine production, cytotoxicity).
Troubleshooting Tips:
- Low editing efficiency: Optimize sgRNA positioning, increase MOI for viral delivery, or test different editor variants.
- High bystander editing: Adjust sgRNA to reposition editing window or use editors with narrower activity windows.
- Reduced cell viability: Lower viral titer, reduce LNP concentration, or shorten exposure time.
Prime Editing Protocol for Precise Genome Correction
This protocol describes the use of prime editing for precise correction of pathogenic mutations in patient-derived iPSCs, incorporating the latest PE6 architecture for enhanced efficiency [55].
Materials Required:
- Prime editor expression plasmid (PE6e recommended for balance of efficiency and specificity)
- Optimized pegRNA with 3'-stabilizing structure (e.g., epegRNA)
- nicking sgRNA for PE3b strategy (when appropriate)
- Patient-derived iPSCs with target mutation
- Stem cell culture reagents (mTeSR Plus, Y-27632 ROCK inhibitor)
- Delivery system (electroporation for iPSCs)
- MLH1dn plasmid (for PE4/5 approaches to suppress MMR)
Step-by-Step Procedure:
pegRNA Design: Design pegRNA with 10-15nt primer binding site (PBS) and 12-18nt RTT encoding the desired edit. Include 3' structural motifs (e.g., evopreQ1) to enhance pegRNA stability. Use computational tools to minimize RNA secondary structures that impair function.
Cell Preparation: Culture iPSCs in mTeSR Plus on Matrigel-coated plates. Passage cells at 70-80% confluence using EDTA-based dissociation. Pre-treat cells with 10μM Y-27632 1 hour before editing to enhance viability.
Editor Delivery by Electroporation: Harvest iPSCs at 80% confluence. Prepare RNP complex by incubating 10μg PE6 protein with 6μg pegRNA and 3μg nicking sgRNA (for PE3b) for 10 minutes at room temperature. Electroporate 1×10^6 cells using Neon Transfection System (1400V, 20ms, 2 pulses). Include MLH1dn plasmid (2μg) for MMR suppression in PE4/5 approaches.
Post-Editing Culture and Analysis: Plate electroporated cells at low density (10,000 cells/cm²) in mTeSR Plus with 10μM Y-27632. Change media after 24 hours to remove ROCK inhibitor. Allow 72-96 hours for editing manifestation before analysis.
Editing Efficiency Assessment: Harvest cells for genomic DNA extraction. Amplify target region with flanking primers (≥100bp on each side). Use next-generation sequencing with unique molecular identifiers to precisely quantify editing efficiency and byproducts.
Clone Isolation and Validation: For therapeutic applications, isolate single-cell clones by FACS sorting into 96-well plates. Expand for 2-3 weeks, then screen by targeted sequencing. Validate homozygous edited clones by Sanger sequencing and off-target assessment through GUIDE-seq or CIRCLE-seq.
Critical Optimization Parameters:
- PBS length optimization (test 10, 13, 15nt)
- RTT length optimization (match to edit complexity)
- Nicking sgRNA positioning (10-30bp from pegRNA nick site)
- MMR suppression timing (co-delivery vs. pre-treatment)
Epigenome Modulation Protocol for Gene Silencing
This protocol details the use of the RENDER platform for durable epigenetic silencing in therapeutic cell types, including primary T-cells and stem cell-derived neurons [57].
Materials Required:
- CRISPRoff epigenome editor (dCas9-DNMT3A-3L-KRAB)
- Target-specific sgRNA (designed for promoter regions)
- HEK293T cells for eVLP production
- Primary T-cells or stem cell-derived neurons
- VSV-G envelope plasmid
- Wild-type gag-pol polyprotein plasmid
- Concentration reagents (PEG-it virus precipitation solution)
Step-by-Step Procedure:
eVLP Production: Seed HEK293T cells at 6×10^6 cells per 10cm dish. After 24 hours, co-transfect with gag-CRISPRoff fusion plasmid (8μg), VSV-G envelope plasmid (4μg), gag-pol plasmid (4μg), and sgRNA plasmid (4μg) using PEI transfection reagent. Harvest supernatant at 48 and 72 hours post-transfection.
eVLP Concentration and Purification: Pool harvested supernatants and clarify by centrifugation (2000×g, 10 minutes). Concentrate eVLPs by PEG-it precipitation according to manufacturer's instructions. Resuspend pellet in 1/100th volume PBS, aliquot, and store at -80°C. Quantify editor packaging by ELISA.
Cell Treatment: For primary T-cells, activate with anti-CD3/CD28 beads for 48 hours prior to treatment. Treat 1×10^6 cells with 100μL concentrated eVLPs in the presence of 8μg/mL polybrene via spinfection (1000×g, 90 minutes, 32°C). For neurons, treat 5×10^4 iPS-derived neurons at day 14 of differentiation without spinfection.
Silencing Validation: Assess epigenetic silencing 7 days post-treatment through: (1) RNA extraction and RT-qPCR for transcript reduction, (2) bisulfite sequencing for promoter methylation analysis, (3) Western blot or flow cytometry for protein-level reduction.
Durability Assessment: Monitor silencing persistence through serial passaging (for dividing cells) or extended culture (for post-mitotic cells). Sample cells weekly for up to 60 days to confirm maintenance of epigenetic marks.
Key Optimization Considerations:
- eVLP concentration: Test 10-200μL per 1×10^6 cells
- sgRNA targeting: Design multiple sgRNAs targeting within ±500bp of transcription start site
- Treatment timing: For dividing cells, treat during active growth phase; for post-mitotic cells, ensure health status pre-treatment
- Multi-locus targeting: Co-package multiple sgRNAs for simultaneous epigenetic regulation of several genes
Table 2: Progression of Prime Editing Systems
| Version | Key Components | Editing Efficiency | Improvements and Applications |
|---|---|---|---|
| PE1 | Nickase Cas9 (H840A) + M-MLV RT | ~10-20% in HEK293T cells | Proof-of-concept for search-and-replace editing [55] |
| PE2 | Nickase Cas9 + improved RT | ~20-40% in HEK293T cells | Enhanced RT processivity and stability [55] |
| PE3 | PE2 + additional sgRNA | ~30-50% in HEK293T cells | Dual nicking increases editing efficiency [55] |
| PE4 | PE2 + MLH1dn | ~50-70% in HEK293T cells | MMR suppression enhances editing efficiency [55] |
| PE5 | PE3 + MLH1dn | ~60-80% in HEK293T cells | Combines dual nicking with MMR inhibition [55] |
| PE6 | Modified RT + epegRNAs | ~70-90% in HEK293T cells | Compact RT variants improve delivery; stabilized pegRNAs [55] |
| PE7 | PE6 + La protein fusion | ~80-95% in HEK293T cells | Enhanced pegRNA stability and editing outcomes [55] |
Visualization of Experimental Workflows
Diagram 1: Comparative experimental workflows for the three advanced editing platforms, highlighting key methodological differences from design to validation.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Reagents for Advanced Editing Platforms
| Reagent Category | Specific Examples | Function & Application Notes |
|---|---|---|
| Editor Plasmids | PE6max (Addgene #174375), ABE8e (Addgene #138495), CRISPRoff v2 (Addgene #167981) | Engineered for enhanced efficiency and specificity; codon-optimized for human cells |
| Delivery Systems | Lentiviral packaging plasmids (psPAX2, pMD2.G), LNP formulations, Neon Transfection System | Match delivery method to cell type: viral for hard-to-transfect, LNP/electroporation for primary cells |
| pegRNA/sgRNA | epegRNA with evopreQ1 motif, Alt-R CRISPR-Cas9 sgRNA | Chemical modifications enhance stability; specialized scaffolds for different editor systems |
| Cell Culture Reagents | mTeSR Plus (iPSCs), X-VIVO 15 (lymphocytes), Y-27632 (ROCK inhibitor) | Optimized media and supplements maintain cell viability during editing process |
| Validation Tools | Illumina DNA Prep kits, TIDE decomposition tool, Bisulfite conversion kits | Multi-modal validation essential: NGS for efficiency, functional assays for outcome |
| Specialized Additives | MLH1dn (MMR suppression), Scr7 (NHEJ inhibitor), L755507 (enhances HDR) | Improve editing outcomes by modulating DNA repair pathways |
| MSN-125 | MSN-125, MF:C36H38BrN3O6, MW:688.6 g/mol | Chemical Reagent |
| Lomefloxacin | Lomefloxacin, CAS:114394-67-1; 98079-51-7; 98079-52-8, MF:C17H19F2N3O3, MW:351.35 g/mol | Chemical Reagent |
The advanced editing platforms of base editing, prime editing, and epigenome modulation represent a transformative toolkit for therapeutic cell design, each offering distinct advantages for specific research and clinical applications. Base editing provides efficient, precise point mutation correction with minimal indel formation; prime editing enables versatile "search-and-replace" editing for diverse sequence changes; and epigenome modulation allows reversible, durable gene regulation without permanent genomic alteration.
The rapid evolution of these technologies continues to address initial limitations through improved editor architectures, enhanced delivery systems, and greater understanding of cellular context effects. As these platforms mature, they promise to accelerate the development of sophisticated cell therapies for genetic disorders, cancer, and degenerative diseases. Researchers are now equipped with an unprecedented ability to precisely manipulate genomic and epigenomic information, opening new frontiers in therapeutic cell engineering.
The advent of CRISPR-Cas genome editing has inaugurated a transformative era in therapeutic cell design, particularly for rare genetic disorders. While conventional drug development approaches often neglect rare diseases due to limited patient populations and economic constraints, CRISPR technology offers a paradigm shift toward personalized, precision genetic medicines. The recent successful application of a fully personalized CRISPR therapy for an infant with a rare metabolic disorder demonstrates the practical realization of this potential, establishing a regulatory and methodological precedent for patient-specific therapies [8] [58]. This breakthrough exemplifies how CRISPR-based therapeutic cell design can address the unique genetic profile of individual patients, moving beyond the "one-size-fits-all" approach that has dominated medicine.
The convergence of advanced CRISPR editing tools, sophisticated delivery systems, and streamlined regulatory pathways has created an unprecedented opportunity to develop bespoke therapies for genetic conditions that were previously considered untreatable. This application note details the experimental protocols, quantitative outcomes, and practical implementation framework for developing patient-specific CRISPR therapies, providing researchers and drug development professionals with actionable methodologies for therapeutic translation. By framing these developments within the broader context of therapeutic cell design research, this document aims to accelerate the adoption of precision genetic medicine approaches for rare diseases.
Breakthrough Case Study: Personalized CRISPR for CPS1 Deficiency
Clinical Context and Therapeutic Strategy
The landmark case involved an infant, designated KJ, diagnosed with carbamoyl phosphate synthetase 1 (CPS1) deficiency, a rare autosomal recessive urea cycle disorder that prevents the normal detoxification of ammonia [58] [59]. Patients with this condition typically require severe protein restriction and medications to manage ammonia levels until they are eligible for liver transplantation, with persistent risk of neurological damage and mortality from metabolic crises [59]. The research team at Children's Hospital of Philadelphia (CHOP) and Penn Medicine developed a bespoke base editing therapy targeting KJ's specific CPS1 mutation, delivering the corrective editing components via lipid nanoparticles (LNPs) to liver cells [58].
This case established several critical precedents: it represented the first fully personalized CRISPR therapy developed for a single patient, demonstrated the feasibility of rapid therapy development (six months from diagnosis to treatment), and validated the safety and efficacy of LNP-mediated in vivo delivery for precise genetic correction [58] [59]. The success of this approach provides a regulatory and methodological template for extending similar strategies to other rare genetic disorders, particularly those affecting solid organs accessible to LNP targeting.
Quantitative Therapeutic Outcomes
The therapeutic intervention yielded quantitatively measurable improvements in both biochemical parameters and clinical outcomes, as summarized in Table 1.
Table 1: Quantitative Outcomes from Personalized CPS1 Deficiency Therapy
| Parameter | Pre-Treatment Status | Post-Treatment Outcome | Timeline |
|---|---|---|---|
| Dietary Protein Tolerance | Severely restricted | Increased tolerance demonstrated | 2-4 weeks post-initial dose |
| Ammonia Control | Medication-dependent | Reduced medication requirements | Sustained through follow-up |
| Illness Resilience | High risk of metabolic crisis | Normal recovery from rhinovirus and GI illness | 1-2 months post-treatment |
| Treatment Safety | N/A | No serious side effects | Across all three doses |
| Editing Efficiency | N/A | Incremental improvement with each dose | Demonstrated through 3 doses |
The patient received three incremental doses of the LNP-formulated base editing therapy, with each subsequent dose increasing the percentage of corrected liver cells without triggering adverse immune reactions or other safety concerns [8] [58]. This redosing capability, facilitated by the non-immunogenic properties of LNPs compared to viral delivery vectors, represents a significant advantage for titrating therapies to achieve therapeutic efficacy while maintaining safety margins.
Experimental Protocols and Methodologies
Therapeutic Design and Development Workflow
The development of patient-specific CRISPR therapies requires an integrated, multidisciplinary approach with carefully coordinated parallel processes. The following protocol outlines the key stages from genetic diagnosis to therapy administration:
Figure 1: Bespoke CRISPR Therapy Development Workflow
Phase 1: Genetic Diagnosis and Target Identification (2-3 weeks)
- Perform whole exome or genome sequencing to identify causative mutation
- Confirm pathogenicity of variant through functional databases and literature review
- Design patient-specific guide RNA (gRNA) with optimal on-target efficiency and minimal off-target potential
- Select appropriate CRISPR system (Cas9, base editor, prime editor) based on required edit type
Phase 2: Therapeutic Construct Assembly (3-4 weeks)
- Clone gRNA sequence into appropriate expression vector
- Incorporate CRISPR machinery into selected delivery platform (LNP formulation preferred for in vivo liver delivery)
- Validate editing efficiency and specificity in relevant cell lines (HEK293T, HepG2)
Phase 3: Preclinical Safety and Efficacy Assessment (6-8 weeks)
- Evaluate off-target editing profiles using CIRCLE-seq or GUIDE-seq
- Assess efficacy in patient-derived iPSCs or animal models when available
- Conduct toxicology studies in relevant animal models
- Establish maximum tolerated dose and therapeutic window
Phase 4: Regulatory Review and cGMP Manufacturing (10-12 weeks)
- Prepare Investigational New Drug (IND) application with accelerated pathway justification
- Manufacture clinical-grade material under cGMP conditions
- Perform quality control testing (potency, purity, sterility)
Phase 5: Clinical Administration and Monitoring
- Administer initial low dose with rigorous safety monitoring
- Titrate subsequent doses based on therapeutic response and safety profile
- Implement long-term surveillance for delayed effects
LNP Formulation and In Vivo Delivery Protocol
Lipid nanoparticles have emerged as the preferred delivery vehicle for in vivo CRISPR therapies targeting the liver due to their natural tropism for hepatic tissue, transient activity profile, and capacity for redosing. The following protocol details LNP formulation for CRISPR component delivery:
Reagents and Equipment:
- Ionizable lipid (e.g., DLin-MC3-DMA)
- Helper lipids (DSPC, cholesterol, DMG-PEG2000)
- CRISPR cargo (mRNA encoding base editor + sgRNA)
- Microfluidic mixer (NanoAssemblr, Precision NanoSystems)
- Dialysis membranes (MWCO 100kDa)
Procedure:
- Prepare lipid mixture in ethanol at precise molar ratios (ionizable lipid:helper lipid:cholesterol:PEG-lipid = 50:10:38.5:1.5)
- Dissolve CRISPR cargo in aqueous citrate buffer (pH 4.0)
- Combine aqueous and ethanol phases using microfluidic mixer at 1:3 flow rate ratio (total flow rate 12 mL/min)
- Dialyze resulting LNP formulation against PBS (pH 7.4) for 24 hours at 4°C
- Concentrate using centrifugal filters to desired concentration
- Sterile filter through 0.22μm membrane
- Characterize LNP size (70-100nm ideal), polydispersity (<0.2), encapsulation efficiency (>90%)
Administration:
- Administer via slow intravenous infusion over 2-4 hours
- Monitor for infusion-related reactions
- Consider premedication with antihistamines or corticosteroids for high sensitivity patients
- Subsequent doses may be administered at 2-4 week intervals based on safety and efficacy markers
Safety Considerations and Genomic Integrity
The therapeutic application of CRISPR technologies requires careful attention to genomic integrity beyond conventional off-target profiling. Recent research has revealed that CRISPR editing can induce structural variations (SVs), including kilobase- to megabase-scale deletions, chromosomal translocations, and complex rearrangements, particularly when DNA repair pathways are manipulated to enhance editing efficiency [62].
Mitigation Strategies for Structural Variations
- Avoid DNA-PKcs inhibitors: The use of DNA-PKcs inhibitors to enhance HDR efficiency markedly increases the frequency of large-scale deletions and chromosomal translocations [62].
- Implement comprehensive SV screening: Employ long-read sequencing and specialized assays (CAST-Seq, LAM-HTGTS) to detect large structural variations that conventional short-read sequencing misses [62].
- Prefer single-dose strategies: Where possible, utilize highly efficient editors that achieve therapeutic benefit without requiring multiple treatments or HDR enhancement [62].
- Monitor p53 pathway activation: Assess p53 response in edited cells, as persistent p53 activation may indicate DNA damage response, while suppression could promote oncogenic transformation [62].
Table 2: Safety Assessment Methods for Bespoke CRISPR Therapies
| Risk Category | Detection Method | Acceptance Criteria |
|---|---|---|
| Off-Target Editing | GUIDE-seq, CIRCLE-seq | No edits in predicted high-risk off-target sites |
| Structural Variations | Long-read sequencing, CAST-Seq | No megabase-scale deletions or translocations |
| On-Target Genotoxicity | Karyotyping, FISH analysis | Normal chromosomal structure and number |
| Immune Response | Cytokine profiling, immunoassays | No significant elevation of pro-inflammatory cytokines |
| Tumorigenicity | p53 pathway activation, transformation assays | No evidence of malignant transformation |
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of bespoke CRISPR therapies requires specialized reagents and platforms optimized for precision and safety. Table 3 details critical components for developing patient-specific gene therapies.
Table 3: Essential Research Reagents for Bespoke CRISPR Therapy Development
| Reagent Category | Specific Examples | Function & Application |
|---|---|---|
| CRISPR Editors | Base editors (ABE, CBE), Prime editors, Cas9-HF1 | Precise genetic correction without double-strand breaks |
| Delivery Systems | Selective Organ Targeting (SORT) LNPs, AAV variants | Tissue-specific delivery of editing components |
| gRNA Design Tools | CRISPRscan, ChopChop, CRISPick | Optimal gRNA selection with off-target prediction |
| Safety Assessment | GUIDE-seq, CIRCLE-seq, CAST-Seq | Comprehensive genomic integrity evaluation |
| Cell Models | Patient-derived iPSCs, Organoids | Disease modeling and therapeutic validation |
| Analytical Methods | ddPCR, NGS amplicon sequencing, LC-MS | Precise quantification of editing outcomes |
| Antiviral agent 55 | Antiviral agent 55, MF:C21H20N2O4, MW:364.4 g/mol | Chemical Reagent |
The successful implementation of personalized CRISPR therapy for CPS1 deficiency represents a paradigm shift in therapeutic cell design, demonstrating that patient-specific genetic medicines can be developed within clinically meaningful timelines. This case establishes a methodological framework that can be adapted to other rare genetic disorders, particularly those affecting the liver and other tissues accessible to nanoparticle delivery.
The integration of advanced delivery platforms like LNPs with precision editing tools such as base editors creates a powerful therapeutic pipeline that balances efficacy with safety. As the field advances, key focus areas will include expanding tissue targeting capabilities, enhancing editing precision through novel editor systems, and streamlining regulatory pathways for personalized therapies. The ongoing development of compact editing systems like Cas12f-based editors and enhanced specificity variants will further expand the therapeutic landscape [7].
For researchers and therapeutic developers, this breakthrough underscores the feasibility of creating bespoke genetic medicines for ultra-rare conditions, transforming what was once theoretical into practical reality. By adopting the protocols, safety assessments, and reagent strategies outlined in this application note, the research community can accelerate the development of personalized CRISPR therapies for the thousands of genetic conditions that currently lack effective treatments.
The therapeutic application of CRISPR-Cas genome editing is fundamentally constrained by the challenge of delivery. Efficient, specific, and safe delivery of CRISPR machinery—whether as DNA, mRNA, or preassembled ribonucleoprotein (RNP) complexes—is paramount for successful genetic modification in therapeutic cell design. While viral vectors have historically dominated this space, concerns regarding immunogenicity, cargo limitations, and long-term transgene expression have accelerated the development of novel non-viral and synthetic delivery platforms [65] [66]. Among these, Lipid Nanoparticles (LNPs), Virus-Like Particles (VLPs), and other enveloped delivery vehicles have emerged as leading technologies capable of addressing these challenges. This application note provides a detailed overview of these three innovative delivery systems, framing them within the context of CRISPR-Cas therapeutics and providing structured quantitative comparisons, detailed experimental protocols, and essential resource guides for research scientists and drug development professionals.
Comparative Analysis of Delivery Platforms
The selection of an appropriate delivery system is a critical determinant in the success of a CRISPR-based therapeutic project. The table below provides a systematic comparison of the key physical, performance, and practical characteristics of LNPs, VLPs, and enveloped viral vectors to inform this decision.
Table 1: Quantitative Comparison of CRISPR-Cas Delivery Vehicle Characteristics
| Characteristic | Lipid Nanoparticles (LNPs) | Virus-Like Particles (VLPs) | Enveloped Viral Vectors (e.g., Lentivirus, VSV-G Pseudotyped) |
|---|---|---|---|
| Typical Cargo Form | mRNA, RNP [67] | RNP (optimally) [68] | DNA, RNA (for lentivirus) [61] |
| Payload Capacity | High (can package large mRNA) [69] | Moderate (can exceed AAV limits) [68] | High (e.g., Lentivirus: ~10 kb) [61] [70] |
| Editing Efficiency (In Vivo) | High in liver with optimized LNPs [67] | Comparable to AAV and LV in disease models [68] | High (long-term expression) [61] |
| Specific Indel Frequency | Up to 90% in HSPCs (ex vivo) [67] | 38% indel frequency shown in RPE/choroid [68] | Varies with serotype and target cell |
| Transience of Activity | Short-lived (days) [70] [69] | Transient (protein delivered directly) [68] | Prolonged (risk of long-term expression) [61] [70] |
| Immunogenicity | Low to moderate [61] | Lower than true viral vectors; evident p24-specific IgG, minimal anti-Cas9 IgG [68] | High (can trigger immune responses) [61] [65] |
| Manufacturing Complexity | Scalable, established for industry [69] | Challenging; scaling is a hurdle [61] [68] | Established but complex |
| Key Advantage | Proven clinical success; transient expression; tunable targeting [61] [69] | Combines high efficiency of viruses with transient activity of RNP; programmable tropism [68] | High transduction efficiency; broad or specific tropism via pseudotyping [61] |
| Key Limitation | Endosomal escape barrier; potential toxicity [61] [70] | Stability and manufacturing challenges [61] | Safety concerns (insertional mutagenesis, immunogenicity) [61] [65] |
Detailed Experimental Protocols
Protocol: Formulation of CRISPR-Cas9 RNP Loaded Lipid Nanoparticles (LNPs) for In Vivo Delivery
This protocol describes the microfluidic formulation of LNPs encapsulating preassembled Cas9-gRNA RNP complexes for high-efficiency in vivo genome editing, adapted from recent literature [70] [67].
I. Materials
- Cas9 Protein: Recombinantly purified, high-concentration stock in a suitable storage buffer (e.g., 20 mM HEPES, 150 mM KCl, 10% Glycerol, pH 7.5).
- sgRNA: Chemically synthesized, target-specific sgRNA, HPLC-purified.
- Lipids: Ionizable cationic lipid (e.g., DLin-MC3-DMA), DSPC (1,2-distearoyl-sn-glycero-3-phosphocholine), Cholesterol, and PEG-lipid (e.g., DMG-PEG 2000).
- Buffers: Ethanol (100%), 1x PBS or 10 mM Citrate buffer (pH 4.0).
- Equipment: Microfluidic mixer (e.g., NanoAssemblr), Syringe pumps, Dialysis cassettes (MWCO 10-20 kDa), Dynamic Light Scattering (DLS) instrument.
II. Methodology
- RNP Complex Formation: Combine Cas9 protein and sgRNA at a molar ratio of 1:1.2 in a nuclease-free assembly buffer. Incubate at room temperature for 10-20 minutes to form the RNP complex.
- Lipid Stock Preparation: Prepare lipid stocks in ethanol. A typical molar ratio is Ionizable lipid:DSPC:Cholesterol:DMG-PEG 2000 = 50:10:38.5:1.5. Adjust ratios based on the specific ionizable lipid used.
- Aqueous Phase Preparation: Dilute the assembled RNP complex into a 10 mM Citrate buffer (pH 4.0) to a final volume equal to the ethanol lipid phase.
- Microfluidic Mixing: Load the lipid-ethanol solution and the RNP-aqueous solution into separate syringes. Set the total flow rate (TFR) to 12 mL/min and a flow rate ratio (FRR) of 3:1 (aqueous:ethanol). Initiate mixing in the microfluidic device.
- Dial Filtration and Buffer Exchange: Immediately collect the LNP suspension and dialyze against a large volume of 1x PBS (pH 7.4) for 4-6 hours at 4°C to remove ethanol and adjust the pH. Alternatively, use tangential flow filtration.
- Characterization and QC:
- Size and PDI: Measure by DLS. Target size: 70-100 nm with PDI < 0.2.
- Encapsulation Efficiency (EE): Quantify using RiboGreen assay. Measure fluorescence of untreated LNPs (background) and LNPs lysed with 1% Triton X-100 (total RNA). Calculate EE% = [1 - (Background/Total)] * 100.
- RNP Integrity: Analyze via agarose or native PAGE gel electrophoresis.
Protocol: Production of Cell-Tropism Programmable VLPs (RIDE System) for RNP Delivery
This protocol outlines the production of the "RIDE" (Rnp Delivery) VLP system, engineered for cell-type-specific delivery of CRISPR-Cas9 RNP, as detailed by [68].
I. Materials
- Plasmids:
- Packaging Plasmid: Encoding GagPol (e.g., with D64V integrase mutation).
- Envelope Plasmid: Encoding VSV-G protein or other targeting envelopes (e.g., CD8 for T cells).
- MS2-Gag Fusion Plasmid: Encoding Gag fused to the MS2 coat protein.
- CRISPR Components Plasmid: Encoding Cas9 protein and the sgRNA scaffold modified with two MS2 stem loops.
- Cell Line: HEK293T cells.
- Media: DMEM with 10% FBS, antibiotics; Opti-MEM reduced serum media.
- Transfection Reagent: Polyethylenimine (PEI MAX).
- Reagents: Benzonase, PEG-it Virus Precipitation Solution, Sucrose for gradient purification, p24 ELISA kit for titering.
II. Methodology
- Cell Seeding and Transfection: Seed HEK293T cells in a 10 cm culture dish to reach 70-80% confluency at the time of transfection. Co-transfect the cells with the four plasmids (Packaging, Envelope, MS2-Gag, and CRISPR Components) using PEI MAX according to manufacturer's instructions.
- VLP Harvest and Clarification: At 48-72 hours post-transfection, collect the cell culture supernatant. Centrifuge at low speed (e.g., 2000 x g for 10 min) to remove cell debris. Filter the supernatant through a 0.45 µm filter.
- VLP Concentration and Purification: Concentrate the clarified supernatant using PEG-it solution overnight at 4°C, followed by centrifugation. For higher purity, resuspend the pellet and purify via sucrose density gradient ultracentrifugation (e.g., 20% sucrose cushion).
- Titering and Quality Control:
- Physical Titer: Quantify VLP concentration using a p24 ELISA kit.
- Functional Titer: Transduce target cells with serial dilutions of VLPs and assess editing efficiency at the genomic target site 72 hours later via T7E1 assay or next-generation sequencing.
- Purity and Structure: Assess by electron microscopy and Western blot for Cas9 and p24.
System Workflows and Signaling Pathways
The following diagrams illustrate the structural configuration and production workflow of the programmable RIDE VLP system, a key innovation in enveloped delivery vehicles.
Diagram Title: RIDE VLP Structure and Production Flow
The Scientist's Toolkit: Research Reagent Solutions
The table below catalogs essential reagents and their functional roles for implementing the delivery protocols described in this note.
Table 2: Essential Research Reagents for Delivery System Implementation
| Reagent / Material | Function / Role | Key Characteristics & Notes |
|---|---|---|
| Ionizable Cationic Lipid (e.g., DLin-MC3-DMA) | Key functional lipid in LNPs; enables nucleic acid/RNP encapsulation and endosomal escape [61] [67]. | Critical for in vivo efficacy. Newer variants (e.g., for SORT nanoparticles) enable organ-specific targeting [61]. |
| DMG-PEG 2000 | Polyethylene glycol (PEG)-lipid used in LNP formulation; confers stability and "stealth" properties; modulates pharmacokinetics [67]. | PEG percentage can be tuned to influence circulation time and targeting. |
| MS2 Coat Protein-Fused Gag | Engineered structural protein for VLPs; specifically binds MS2 stem loops on gRNA to package preassembled Cas9 RNP [68]. | Core component of the RIDE system; enables specific RNP loading over nucleic acids. |
| MS2 Stem Loop-Modified gRNA | Modified guide RNA; serves as a "handle" for VLP packaging via interaction with MS2-Gag fusion protein [68]. | Maintains full guide activity for Cas9 targeting while enabling efficient VLP packaging. |
| VSV-G Envelope Protein | Commonly used envelope for pseudotyping both LV and VLP systems; confers broad tropism by binding to LDL receptors [61] [68]. | Can be substituted with cell-specific targeting envelopes (e.g., from CD8, CD4) for programmable tropism [68]. |
| Benzonase Nuclease | Enzyme added during VLP purification; degrades unpackaged nucleic contaminants, improving safety and purity [68]. | Reduces carry-over of plasmid DNA, minimizing potential immune activation and confounding results. |
| Polyethylenimine (PEI MAX) | Cationic polymer transfection reagent; standard for transient co-transfection of multiple plasmids in HEK293T cells for VLP/Virus production [68]. | Cost-effective for research-scale production; can be optimized for specific cell lines and plasmid sizes. |
| p24 ELISA Kit | Immunoassay for quantifying the concentration of the lentiviral/ VLP capsid protein p24; used for determining physical particle titer [68]. | Essential for standardizing doses across experiments in transductions. |
Navigating Technical Hurdles: Safety, Efficiency, and Clinical Translation Challenges
In the field of therapeutic cell design, the precision of CRISPR-Cas genome editing is paramount. Off-target effects—unintended modifications at genomic sites similar to the target sequence—represent a significant safety concern that can compromise experimental validity and clinical safety [71] [72]. These effects arise primarily from the tolerance of Cas nucleases for mismatches between the guide RNA (gRNA) and genomic DNA, particularly outside the seed region proximal to the Protospacer Adjacent Motif (PAM) [72]. As CRISPR-based therapies advance through clinical trials, with milestones such as the approval of Casgevy for sickle cell disease, the rigorous assessment and mitigation of off-target activity has become a regulatory imperative [8] [73]. This document provides a comprehensive technical overview of contemporary detection methodologies and engineered high-fidelity Cas variants, providing researchers with practical frameworks for enhancing editing specificity in therapeutic development.
Detection Methods for Off-Target Effects
A critical component of therapeutic CRISPR development is the comprehensive profiling of off-target activity. Detection methods span computational prediction, in vitro biochemical assays, cell-based methods, and in vivo techniques, each with distinct advantages and limitations. The table below summarizes the key characteristics of major detection methodologies.
Table 1: Comparison of Major Off-Target Detection Methods
| Method | Principle | Advantages | Limitations | Therapeutic Application Context |
|---|---|---|---|---|
| In Silico Prediction (e.g., CRISOT, Cas-OFFinder) [71] [74] | Computational scanning of reference genomes for sequences homologous to gRNA. | Fast, inexpensive; ideal for initial gRNA screening. | Biased toward sgRNA-dependent effects; overlooks cellular context (e.g., chromatin accessibility). | Preliminary gRNA selection and risk assessment during early R&D. |
| Cell-Free Methods (e.g., CIRCLE-seq, Digenome-seq) [71] | In vitro cleavage of purified genomic DNA or cell-free chromatin by Cas9-gRNA RNP complexes, followed by sequencing. | Highly sensitive; controlled environment; no cellular toxicity concerns. | May not fully recapitulate intracellular conditions (e.g., nuclear factors, chromatin structure). | Highly sensitive off-target profiling for lead gRNA candidates prior to cellular testing. |
| Cell Culture-Based Methods (e.g., GUIDE-seq) [71] | Capturing double-strand breaks (DSBs) in living cells via integration of double-stranded oligodeoxynucleotides (dsODNs). | Highly sensitive; low false positive rate; works in relevant cellular environments. | Limited by transfection efficiency; can be challenging in hard-to-transfect primary cells. | Gold standard for definitive off-target profiling in clinically relevant cell models. |
| In Vivo Detection (e.g., DISCOVER-seq) [71] | Utilizes DNA repair proteins (e.g., MRE11) as bait for chromatin immunoprecipitation (ChIP-seq) in vivo. | Captures editing in a physiological context; can detect off-targets in animal models or human patients. | Can have false positives; technically complex and lower resolution. | Assessing off-target effects in pre-clinical animal models or patient samples. |
Experimental Protocol: Genome-Wide Off-Target Screening with GUIDE-seq
GUIDE-seq (Genome-wide Unbiased Identification of DSBs Enabled by Sequencing) is a highly sensitive method for detecting off-target cleavage in cell cultures [71]. Below is a detailed protocol for its implementation.
Reagents and Equipment:
- Cultured mammalian cells (e.g., HEK293T, primary T-cells for therapy)
- Cas9 protein and synthetic sgRNA complexed as Ribonucleoprotein (RNP)
- GUIDE-seq dsODN tag (5'-phosphorylated, 5'-biotin-modified, 34 bp)
- Transfection reagent (e.g., Lipofectamine CRISPRMAX for cell lines or Neon Electroporation system for primary cells)
- Genomic DNA extraction kit
- Covaris sonicator or nebulizer
- Streptavidin-conjugated magnetic beads
- NGS library preparation kit and sequencer
Procedure:
- Transfection: Co-deliver the pre-complexed Cas9-sgRNA RNP and GUIDE-seq dsODN tag into approximately 500,000 cells using an appropriate transfection method. Optimize the ratio of RNP to dsODN (a typical starting point is 2 µg of RNP and 100 pmol of dsODN per sample).
- Genomic DNA Extraction: Incubate cells for 48-72 hours post-transfection to allow for DSB repair and tag integration. Harvest cells and extract high-molecular-weight genomic DNA using a commercial kit.
- DNA Shearing: Fragment the genomic DNA to an average size of 300-500 bp using a Covaris sonicator.
- Tag Enrichment: Incubate the sheared DNA with streptavidin magnetic beads to enrich for fragments containing the integrated biotinylated dsODN tag.
- NGS Library Preparation: Prepare a sequencing library directly from the bead-bound, tag-containing fragments. This typically involves end-repair, adapter ligation, and PCR amplification.
- Sequencing and Data Analysis: Perform high-throughput sequencing (e.g., Illumina MiSeq). Analyze the data using the available GUIDE-seq software pipeline to map all DSB sites, identifying both on-target and off-target integrations.
Figure 1: GUIDE-seq Experimental Workflow. This diagram outlines the key steps for identifying CRISPR off-target effects genome-wide in living cells.
High-Fidelity Cas Variants
To address the inherent specificity challenges of wild-type Cas9, protein engineering has yielded numerous high-fidelity variants with enhanced discrimination against mismatched targets.
Table 2: Comparison of High-Fidelity Cas9 Variants
| Variant | Engineering Strategy | Key Mutations | Specificity Improvement | Considerations for Therapeutic Use |
|---|---|---|---|---|
| eSpCas9 [72] | Rational design to re-establish energetic penalties for mismatches. | K848A, K1003A, R1060A | ~10-fold reduction in off-targets with minimal impact on on-target efficiency. | Widely validated; good balance of high specificity and robust on-target activity. |
| SpCas9-HF1 [72] | Structure-guided rational design to disrupt non-specific interactions with the DNA phosphate backbone. | N497A, R661A, Q695A, Q926A | >85% reduction in off-target activity at tested sites. | Can exhibit reduced on-target efficiency for some gRNAs; requires validation. |
| HiFi Cas9 [75] | Directed evolution to select for variants with improved specificity. | R691A | High on-target efficiency with significantly reduced off-target effects. | Developed by Intellia Therapeutics; shows excellent performance in clinical-grade editing. |
| OpenCRISPR-1 [9] | De novo AI-based design using a protein language model trained on 1 million+ CRISPR operons. | 400+ mutations from SpCas9 | Comparable or improved specificity relative to SpCas9, with high compatibility with base editing. | AI-generated; represents a novel class of editors not constrained by natural evolution. |
Protocol: Validating High-Fidelity Cas Variants
This protocol outlines a standard workflow for comparing the performance of a high-fidelity Cas variant against wild-type SpCas9 in a therapeutically relevant cell model.
Reagents and Equipment:
- High-fidelity Cas9 expression vector (e.g., eSpCas9, HiFi Cas9)
- Wild-type SpCas9 expression vector (positive control)
- sgRNA expression vectors or synthetic gRNAs for 3-5 target loci
- Clinically relevant cell line (e.g., HEK293T, K562, or primary human T-cells)
- Transfection or electroporation system
- Genomic DNA extraction kit
- NGS platform and resources for targeted amplicon sequencing
Procedure:
- Experimental Setup: For each target locus, transfect cells with the high-fidelity Cas variant, the wild-type Cas9 control, and a no-editor control. Use the same sgRNA and delivery method for all conditions.
- Harvest and Extract DNA: Allow 72 hours for editing to occur, then harvest cells and extract genomic DNA.
- On-Target Efficiency Assessment:
- Design PCR primers to amplify a ~300-500 bp region surrounding each on-target site.
- Generate amplicon NGS libraries and sequence at high depth (>100,000x coverage).
- Use a change-detection tool (e.g., CRISPResso2) to quantify insertion/deletion (indel) frequencies at each on-target site.
- Off-Target Assessment:
- Select 10-15 potential off-target sites for each gRNA using an in silico tool (e.g., CRISOT [74] or Cas-OFFinder).
- Perform targeted amplicon sequencing on these sites.
- Quantify any indels at these loci. GUIDE-seq can be performed for a comprehensive, unbiased comparison if resources allow.
- Data Analysis:
- Calculate the ratio of on-target efficiency (High-Fidelity Cas9 / Wild-type Cas9). A ratio of >0.8 is generally acceptable.
- For each gRNA, note the number and frequency of off-target sites detected above background (e.g., >0.1% indel frequency). A successful high-fidelity variant should show a significant reduction or elimination of these events.
Figure 2: High-Fidelity Cas Variant Validation. This workflow outlines the key steps for benchmarking the performance of a high-fidelity Cas nuclease against wild-type SpCas9.
Successful implementation of the protocols above requires access to specific reagents, computational tools, and commercial resources.
Table 3: Essential Research Reagent Solutions
| Item | Function/Description | Example Providers/Sources |
|---|---|---|
| Synthetic sgRNA | Chemically modified guide RNAs can enhance stability and reduce off-target effects [75]. Modifications (e.g., 2'-O-methyl) are critical for in vivo applications. | Synthego, IDT, Dharmacon |
| High-Fidelity Cas9 Expression Plasmids | DNA or mRNA encoding engineered Cas variants with improved specificity. | Addgene (for research plasmids), Thermo Fisher, Takara Bio |
| CRISPR RNP Kits | Pre-complexed Cas9 protein and sgRNA complexes for direct delivery. Reduces off-target risks by shortening editing window [75]. | Synthego, IDT, Thermo Fisher |
| Off-Target Prediction Software | In silico tools to nominate potential off-target sites for a given sgRNA. CRISOT uses MD simulations for high accuracy [74]. | CRISOT Web Tool, Cas-OFFinder, CRISPOR |
| NGS-Based Off-Target Detection Kits | Commercial kits that simplify workflows like GUIDE-seq or CIRCLE-seq. | Takara Bio (GUIDE-seq Kit), various NGS library prep providers |
| Analysis Software (ICE) | Tool for Inference of CRISPR Edits; analyzes Sanger or NGS data to quantify on-target and off-target editing efficiency [75]. | Synthego ICE Tool (web-based) |
The safe and effective application of CRISPR-Cas genome editing in therapeutic cell design hinges on the meticulous control of off-target effects. As outlined in this document, researchers now have access to a powerful toolkit that combines sophisticated, genome-wide detection methods like GUIDE-seq with a growing arsenal of engineered and AI-designed high-fidelity Cas variants [71] [9]. The integration of computational prediction, careful experimental validation, and the use of optimized reagents provides a robust framework for de-risking therapeutic development. Adhering to these application notes and protocols will empower scientists and drug development professionals to advance the next generation of precise and safe CRISPR-based cell therapies.
The therapeutic application of CRISPR-Cas genome editing represents a paradigm shift in therapeutic cell design, yet its clinical translation remains critically dependent on overcoming fundamental delivery obstacles. Efficient delivery must accomplish multiple objectives: transporting large molecular cargoes across cellular membranes, achieving cell-type specificity, maintaining editing efficiency, and ensuring high safety profiles with minimal off-target effects [76] [77]. No universal delivery method exists; instead, researchers must select from a rapidly evolving toolkit of viral and non-viral strategies, each with distinct advantages and limitations for specific therapeutic contexts.
The choice of delivery system profoundly influences the safety, efficiency, and specificity of genome editing outcomes in target cells. Viral vectors offer high transduction efficiency but present safety concerns including immunogenicity and insertional mutagenesis, while non-viral methods provide improved safety profiles but often require optimization for specific cell types [77] [61]. This application note examines the primary cell-specific barriers to CRISPR delivery and provides detailed protocols for implementing optimized strategies in therapeutic development pipelines.
Analysis of Key Delivery Barriers
Cargo-Specific Delivery Challenges
The molecular format of CRISPR components significantly impacts delivery efficiency and editing outcomes. Each cargo type presents distinct challenges for cellular delivery and persistence.
Table 1: CRISPR Cargo Formats and Their Characteristics
| Cargo Format | Size Considerations | Persistence in Cell | Key Challenges | Ideal Use Cases |
|---|---|---|---|---|
| Plasmid DNA | Large size (>9kb for SpCas9) | Prolonged expression increases off-target risk | Cytotoxicity, variable editing efficiency, immunogenicity | Applications requiring sustained editor expression |
| mRNA | Smaller than DNA, requires nuclear export | Transient (days) | Rapid degradation, requires efficient RNP assembly | Reduced off-target editing, transient expression needs |
| Ribonucleoprotein (RNP) | Immediate activity, no transcription/translation needed | Most transient (hours) | Large size (~160kDa Cas9+sgRNA), delivery efficiency | Highest precision, minimal off-target effects, clinical applications |
Cell-Specific Intracellular Barriers
Different cell types present unique barriers that impede efficient CRISPR delivery. The journey from extracellular space to the nucleus involves navigating multiple obstacles that vary across cell types and delivery methods.
The critical path to successful intracellular delivery involves navigating multiple barriers. Extracellularly, CRISPR cargo must avoid immune recognition and serum degradation. Cell entry depends on receptor availability and membrane composition, which varies significantly between cell types. Following endocytosis, the cargo must escape endosomes before lysosomal degradation occurs—a particularly critical barrier for non-viral delivery systems. Finally, the cargo must traverse the nuclear envelope through nuclear pore complexes, with efficiency varying based on cargo size and format and being particularly challenging in non-dividing cells [77] [61].
Delivery Vehicle Optimization Strategies
Viral Vector Engineering
Viral vectors remain among the most efficient delivery vehicles, with specific serotypes optimized for different target cell types.
Table 2: Viral Vector Comparison for Cell-Specific Delivery
| Vector Type | Packaging Capacity | Primary Target Cells | Key Advantages | Safety Concerns |
|---|---|---|---|---|
| AAV | <4.7 kb | Retinal cells, skeletal muscle, liver, CNS | Low immunogenicity, high tissue specificity, long-term expression | Limited cargo capacity, pre-existing immunity |
| Lentivirus | ~8 kb | Hematopoietic cells, immune cells, stem cells | Infects dividing and non-dividing cells, stable integration, high titer | Insertional mutagenesis, oncogenesis risk |
| Adenovirus | Up to 36 kb | Respiratory epithelial cells, dendritic cells | Large cargo capacity, high transduction efficiency, no integration | Strong immune response, inflammation |
| Virus-Like Particles (VLPs) | Variable | Customizable targeting | Non-integrating, reduced immunogenicity, transient expression | Manufacturing complexity, stability issues |
Non-Viral Delivery Optimization
Non-viral delivery methods have gained prominence due to their favorable safety profiles and reduced immunogenicity.
Lipid Nanoparticles (LNPs) have emerged as particularly promising vehicles, especially for hepatic delivery. Their composition can be tuned for specific cell types through Selective Organ Targeting (SORT) technology. LNPs naturally accumulate in the liver but can be engineered to target other tissues by incorporating supplemental molecules that alter their surface properties and tropism [8] [61].
Extracellular Vesicles (EVs) represent another promising non-viral approach, offering natural membrane composition derived from donor cells that can be engineered for enhanced homing to specific tissues. However, challenges remain in standardizing EV production and achieving consistent cargo loading [76] [61].
Experimental Protocols
Protocol: LNP-Mediated RNP Delivery to Hepatocytes
This protocol details an optimized method for delivering CRISPR RNP complexes to hepatocytes using LNPs, based on successful clinical approaches for liver-directed editing [8].
Materials:
- Ionizable cationic lipids (e.g., DLin-MC3-DMA)
- Helper lipids (DSPC, cholesterol, PEG-lipid)
- Cas9 protein with nuclear localization signal
- Synthetic sgRNA
- Microfluidic mixer
- Dialysis membranes (MWCO 100 kDa)
- HepG2 cells or primary hepatocytes
Procedure:
- RNP Complex Formation: Incubate Cas9 protein with sgRNA at 3:1 molar ratio in nuclease-free buffer for 10 minutes at room temperature
- LNP Formulation: Prepare lipid mixture in ethanol at following molar ratios:
- Ionizable lipid: 50%
- Cholesterol: 38.5%
- DSPC: 10%
- PEG-lipid: 1.5%
- Encapsulation: Mix lipid solution with RNP complex in acetate buffer (pH 4.0) using microfluidic device at 3:1 aqueous-to-ethanol flow rate ratio
- Buffer Exchange: Dialyze formed LNPs against PBS (pH 7.4) for 4 hours at 4°C to remove ethanol and establish neutral pH
- Characterization: Measure particle size (target: 80-100 nm) by dynamic light scattering and encapsulation efficiency by RiboGreen assay
- Cell Treatment: Incubate hepatocytes with LNP-RNP complexes at 0.5-1.0 μg/μL Cas9 concentration for 24 hours in serum-free media
- Analysis: Harvest cells 72 hours post-treatment and assess editing efficiency by T7E1 assay or next-generation sequencing
Troubleshooting:
- Low editing efficiency: Optimize RNP:LNP ratio or increase incubation time
- High cytotoxicity: Reduce LNP concentration or shorten exposure time
- Poor encapsulation: Adjust flow rate ratio during microfluidic mixing
Protocol: rAAV Delivery with Compact Cas Variants
This protocol describes the use of recombinant AAV with compact Cas orthologs to overcome packaging limitations, enabling efficient in vivo delivery [78].
Materials:
- Compact Cas ortholog (e.g., SaCas9, CjCas9, Cas12f)
- AAV transfer plasmid with tissue-specific promoter
- AAV helper plasmid
- Packaging cells (HEK293T)
- Polyethylenimine (PEI) transfection reagent
- Iodixanol gradient solutions
Procedure:
- Vector Design: Clone compact Cas gene and sgRNA expression cassette into AAV transfer plasmid (total size <4.7 kb)
- Virus Production: Co-transfect HEK293T cells with:
- AAV transfer plasmid
- AAV rep/cap plasmid (select serotype for tissue tropism)
- Adenoviral helper plasmid Use PEI at 3:1 PEI:DNA ratio in serum-free media
- Harvest and Purify: Collect cells 72 hours post-transfection, lyse by freeze-thaw, treat with benzonase, and purify by iodixanol gradient ultracentrifugation
- Titration: Quantify viral genome copies by qPCR with ITR-specific primers
- In Vivo Delivery: Administer via route appropriate for target tissue:
- Liver: 1×10^12 - 1×10^13 vg/mouse via tail vein injection
- Brain: 1×10^10 - 1×10^11 vg/mouse via stereotactic injection
- Muscle: 1×10^10 - 1×10^11 vg/mouse via intramuscular injection
- Analysis: Assess editing efficiency 2-4 weeks post-injection by sequencing target locus
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for CRISPR Delivery Optimization
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Viral Packaging Systems | AAVpro Helper Free System (Takara), Lenti-X Packaging Single Shots (Clontech) | Production of high-titer viral vectors | Select serotype based on target cell tropism; AAV-DJ enables broad tropism |
| Lipid Nanoparticles | GenCRISPR LNP Kit (Sigma), Invivofectamine 3.0 (Thermo Fisher) | Non-viral encapsulation and delivery | Optimize lipid:RNA ratio for each cell type; use SORT molecules for tissue targeting |
| Cas9 Protein | Alt-R S.p. Cas9 Nuclease V3 (IDT), TrueCut Cas9 Protein (Thermo Fisher) | RNP complex formation | Use high-purity, endotoxin-free grade for sensitive primary cells |
| Modified sgRNAs | Alt-R CRISPR-Cas9 sgRNA (IDT), Synthego sgRNA EZ Kit | Guide RNA with enhanced stability | Chemical modifications (2'-O-methyl, phosphorothioate) improve nuclease resistance |
| Editing Detection | T7 Endonuclease I, Alt-R Genome Editing Detection Kit (IDT), ICE Analysis Tool (Synthego) | Quantification of editing efficiency | T7E1 for quick assessment; NGS for comprehensive analysis including off-targets |
Safety Considerations and Validation
As CRISPR therapies advance toward clinical application, comprehensive safety validation becomes paramount. Recent studies have revealed that CRISPR editing can generate unexpected large-scale structural variations (SVs), including chromosomal translocations and megabase-scale deletions, particularly when DNA-PKcs inhibitors are used to enhance HDR efficiency [62].
Essential Safety Assessments:
- Structural Variation Analysis: Employ long-read sequencing (Oxford Nanopore, PacBio) or specialized methods (CAST-Seq, LAM-HTGTS) to detect large deletions and rearrangements missed by short-read sequencing
- Off-Target Profiling: Use GUIDE-seq or CIRCLE-seq for unbiased genome-wide off-target detection
- p53 Response Monitoring: Assess p53 activation post-editing, as transient p53 suppression may reduce chromosomal aberrations but raises oncogenic concerns in the long term [62]
Risk Mitigation Strategies:
- Avoid DNA-PKcs inhibitors in therapeutic contexts when possible
- Implement rigorous clone screening with multiple verification methods
- Utilize high-fidelity Cas variants (e.g., HiFi Cas9) to reduce off-target activity while recognizing that on-target aberrations may still occur
The landscape of CRISPR delivery is rapidly evolving, with no single solution addressing all cell-specific barriers. Successful therapeutic cell design requires meticulous matching of delivery strategy to target cell type, considering cargo format, vehicle properties, and intended therapeutic outcome. Viral vectors offer efficiency for accessible tissues, while advancing LNP technologies enable precise non-viral delivery. As the field progresses, integrating comprehensive safety assessment protocols will be crucial for translating promising delivery strategies into safe, effective therapies. The continued development of cell-specific delivery platforms will undoubtedly expand the therapeutic reach of CRISPR genome editing in the coming years.
The Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR)-Cas system has revolutionized therapeutic cell design, yet the immunogenicity of bacterial-derived Cas nucleases presents a significant translational challenge. Pre-existing immunity to Cas proteins exists in a substantial proportion of the human population due to previous exposure to the bacteria from which these proteins originate, most commonly Streptococcus pyogenes (SpCas9) and Staphylococcus aureus (SaCas9). This immune memory can trigger both humoral and cellular responses against CRISPR-based therapies, potentially compromising treatment efficacy and safety [79].
Immunological recognition of Cas9 can initiate both innate and adaptive immune responses. The complex interactions between Cas9, delivery vectors, and host immune reactivity play a crucial role in determining the safety and efficacy of CRISPR-based treatments [80]. For researchers engineering therapeutic cells, understanding and addressing these immune responses is paramount for successful clinical application, particularly for in vivo editing strategies where Cas9 expression occurs in the presence of a fully functional immune system.
Prevalence and Mechanisms of Preexisting Immunity
Epidemiology of Cas-Directed Immunity
Seroprevalence studies demonstrate that preexisting immunity to Cas proteins is widespread in the human population. An analysis of 34 donor blood samples revealed IgG antibodies against SaCas9 in 79% of samples and against SpCas9 in 65% of samples [79]. Cellular immunity data from the same study indicated T-cell responses to SaCas9 in 46% of donors, though the sensitivity limitations of the assay may underestimate responses to SpCas9 [79]. These findings indicate that the majority of the potential patient population has some degree of pre-sensitization to commonly used Cas orthologs.
Table 1: Preexisting Immunity to Common Cas Proteins in Human Populations
| Cas Protein | Source Bacterium | Antibody Prevalence | T-cell Prevalence | Clinical Implications |
|---|---|---|---|---|
| SpCas9 | Streptococcus pyogenes | 65% | Potentially underdetected | Risk of antibody-mediated clearance of vectors or Cas-expressing cells |
| SaCas9 | Staphylococcus aureus | 79% | 46% | Cytotoxic T-cell-mediated elimination of edited cells |
| Novel/Engineered Cas | Various (AI-designed) | Unknown, likely lower | Unknown, likely lower | Reduced preexisting immunity; requires validation |
Immunological Mechanisms
The adaptive immune response to Cas proteins involves both antibody-mediated (humoral) and T-cell-mediated (cellular) components. Antibodies against Cas9 can opsonize viral vectors or Cas9-expressing cells, potentially leading to their clearance by phagocytic cells [79]. However, the more significant concern for durable therapeutic effects is cellular immunity, specifically CD8+ cytotoxic T lymphocytes (CTLs) that can recognize and eliminate cells expressing Cas9 proteins [79].
The initial trigger for immune responses involves Cas9 epitope presentation by major histocompatibility complex (MHC) molecules. Antigen-presenting cells process Cas9 proteins and present peptides on MHC class I and II molecules, activating both CD8+ and CD4+ T cells, respectively. For CRISPR-based therapeutics, this becomes particularly problematic when CTLs recognize and destroy the very cells that have been therapeutically edited, thus reversing the potential benefit [79].
Figure 1: Immunological Pathways in Cas9 Immune Recognition. This diagram illustrates how Cas9 proteins trigger both cellular and humoral immune responses that can target therapeutically edited cells for destruction.
Detection and Assessment Methods
Experimental Protocols for Immune Detection
Protocol 3.1.1: Assessing Preexisting Humoral Immunity to Cas Proteins
Purpose: To detect and quantify preexisting anti-Cas9 antibodies in human serum samples.
Materials:
- Recombinant Cas9 protein (SpCas9, SaCas9, or other variants)
- ELISA plates and reagents
- Human serum samples
- Anti-human IgG-HRP conjugate
- TMB substrate and stop solution
- Plate reader
Procedure:
- Coat ELISA plates with 100 µL of recombinant Cas9 protein (1 µg/mL) in carbonate-bicarbonate buffer overnight at 4°C.
- Block plates with 200 µL of 5% non-fat milk in PBST for 2 hours at room temperature.
- Add 100 µL of diluted human serum samples (1:100 in blocking buffer) to wells in triplicate, incubate for 2 hours.
- Wash plates 5 times with PBST.
- Add 100 µL of anti-human IgG-HRP conjugate (1:5000 dilution), incubate for 1 hour.
- Wash plates 5 times with PBST.
- Develop with 100 µL TMB substrate for 15 minutes, then stop with 50 µL 1M H₂SO₄.
- Measure absorbance at 450 nm within 30 minutes.
- Calculate titers relative to standard curve or positive control.
Interpretation: Samples with absorbance values exceeding the mean + 3SD of negative controls are considered seropositive [79].
Protocol 3.1.2: Detection of Cas9-Specific T-cell Responses
Purpose: To identify and quantify Cas9-reactive T cells in human peripheral blood.
Materials:
- Fresh or cryopreserved PBMCs from human donors
- Cas9 protein or overlapping peptide pools
- Positive control (anti-CD3/CD28 beads)
- Negative control (DMSO)
- ELISpot plates or flow cytometry reagents
- IFN-γ capture and detection antibodies (for ELISpot)
- Cell culture medium with 10% human AB serum
Procedure:
- Isolate PBMCs from whole blood using Ficoll density gradient centrifugation.
- For ELISpot: Coat plates with anti-IFN-γ capture antibody overnight, then block with culture medium.
- Seed 2-4×10ⵠPBMCs per well in triplicate.
- Stimulate with Cas9 protein (10 µg/mL) or peptide pools (1 µg/mL per peptide).
- Include positive control (anti-CD3/CD28 beads) and negative control (medium alone).
- Incubate for 40-48 hours at 37°C, 5% CO₂.
- For ELISpot: Develop according to manufacturer's protocol, count spots using automated reader.
- For intracellular cytokine staining: Add brefeldin A after 2 hours, incubate 4-6 more hours, then stain for CD3, CD4, CD8, and IFN-γ for flow cytometry analysis.
Interpretation: Responses are considered positive if the mean spot count or percentage of cytokine-positive T cells exceeds negative control by at least 2-fold and the difference is statistically significant (p < 0.05) [79].
Research Reagent Solutions
Table 2: Essential Reagents for Assessing Cas Protein Immunogenicity
| Reagent Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| Recombinant Cas Proteins | SpCas9, SaCas9, LbCas12a, engineered variants | Antigen for immune assays | Ensure proper folding and purity; test multiple lots |
| Peptide Libraries | Overlapping 15-mer peptides covering full Cas sequence | T-cell epitope mapping | Typically pooled by protein domain for initial screening |
| Detection Antibodies | Anti-human IgG, IgA, IgM; anti-IFN-γ, IL-2, TNF-α | Measuring immune responses | Validate for specific assay format (ELISA, ELISpot, flow) |
| Immune Cell Isolation Kits | PBMC isolation, CD4+/CD8+ T-cell enrichment | Sample preparation | Maintain cell viability and function |
| Antigen-Presenting Cells | Monocyte-derived dendritic cells, B-cell lines | In vitro T-cell stimulation | Match HLA types when possible |
| MHC Multimers | Tetramers, pentamers with Cas9 peptides | Direct detection of antigen-specific T cells | Requires prior epitope identification |
Strategies to Overcome Cas Protein Immunogenicity
Cas Protein Engineering Approaches
Epitope Deletion and Masking
Rational engineering of Cas proteins to remove immunodominant epitopes represents a promising strategy to evade immune recognition. Recent advances have enabled precise identification and modification of immunogenic regions within Cas nucleases. Using mass spectrometry, researchers have identified specific short sequences (approximately eight amino acids long) in both SpCas9 and SaCas12 that trigger immune responses [81]. Computational protein design tools can then generate modified versions that eliminate these immunogenic sequences while preserving editing function.
Protocol 4.1.1: Computational Design of Low-Immunogenicity Cas Variants
Purpose: To engineer Cas proteins with reduced immunogenicity while maintaining editing efficiency.
Materials:
- Sequence and structural data for Cas protein of interest
- Mass spectrometry data identifying immunogenic peptides
- Protein structure prediction software (AlphaFold2, Rosetta)
- Cell lines for functional testing
- Immune detection assays (as described in Section 3.1)
Procedure:
- Identify immunogenic epitopes using mass spectrometry of Cas proteins processed by antigen-presenting cells [81].
- Map these epitopes to the Cas protein structure to determine surface accessibility and functional importance.
- Use computational protein design tools to generate variants that eliminate immunogenic sequences through:
- Conservative amino acid substitutions
- Glycosylation to mask epitopes
- Conformational stabilization to reduce proteasomal processing
- Screen designed variants for:
- Structural stability (molecular dynamics simulations)
- Catalytic activity (in silico docking with DNA and guide RNA)
- PAM recognition maintenance
- Express top candidates and validate experimentally:
- In vitro cleavage assays
- Editing efficiency in relevant cell types
- Reduced immunogenicity in assays from Section 3.1
Validation: The engineered enzymes should demonstrate similar gene-editing efficiency with significantly reduced immune responses compared to wild-type nucleases in both human cells and appropriate animal models [81].
AI-Guided Protein Design
Artificial intelligence approaches now enable the generation of novel Cas proteins with minimal sequence similarity to naturally occurring variants, thereby reducing cross-reactivity with preexisting immunity. Large language models trained on diverse CRISPR operons can generate functional Cas proteins that are hundreds of mutations away from natural sequences [9]. One such AI-generated editor, OpenCRISPR-1, exhibits less than 40% sequence identity to natural Cas9 proteins while maintaining high editing activity and specificity [9].
Figure 2: AI-Guided Engineering of Cas Proteins with Reduced Immunogenicity. This workflow illustrates how artificial intelligence expands the diversity of Cas proteins beyond natural sequences to create editors with potentially reduced immune recognition.
Delivery and Administration Strategies
Optimized Delivery Methods
The method of Cas9 delivery significantly influences immunogenicity outcomes. Table 3 compares delivery approaches and their immunological implications:
Table 3: Delivery Methods and Their Impact on Cas9 Immunogenicity
| Delivery Method | Cas9 Expression Kinetics | Immune Exposure | Advantages | Limitations |
|---|---|---|---|---|
| mRNA/LNP | Transient (days) | Moderate | Self-limiting; reduced chance of sustained immune activation | Still triggers innate immune sensors |
| Protein/RNP | Very short (hours) | Low | No DNA integration; rapid clearance | Lower editing efficiency in some cell types |
| AAV Vector | Long-term (months-years) | High | High transduction efficiency | Sustained antigen presentation increases immunogenicity risk |
| Lentiviral Vector | Long-term (integration) | High | Stable expression; good for ex vivo | Insertional mutagenesis risk; immunogenicity concerns |
| Non-viral DNA | Intermediate (weeks) | Moderate | Easier production; large cargo capacity | Transfection efficiency variable |
Immunosuppressive Protocols
Protocol 4.2.2: Transient Immunosuppression for In Vivo CRISPR Therapies
Purpose: To mitigate anti-Cas9 immune responses during critical periods of Cas9 expression.
Materials:
- Corticosteroids (e.g., methylprednisolone)
- T-cell inhibitors (e.g., tacrolimus)
- mTOR inhibitors (e.g., sirolimus)
- Appropriate animal model or clinical subjects
- Immune monitoring assays
Procedure:
- Initiate immunosuppression 24-48 hours before Cas9 administration.
- Use a combination approach targeting both T-cell activation and cytokine production:
- Corticosteroids: 1-2 mg/kg/day (methylprednisolone equivalent)
- Tacrolimus: Target trough level 5-10 ng/mL
- Sirolimus: Target trough level 5-10 ng/mL
- Maintain immunosuppression for 2-4 weeks based on Cas9 expression kinetics.
- Taper medications over 1-2 weeks while monitoring for immune activation.
- Assess efficacy through:
- Persistence of edited cells
- Absence of anti-Cas9 T-cell expansion
- Clinical markers of therapeutic effect
Considerations: The specific regimen should be tailored to the delivery method, target tissue, and patient population. Liver-directed therapies may require less immunosuppression due to the tolerogenic nature of this organ [79].
Alternative Approaches: Hypoimmune Strategies
Engineering Immune-Evasive Cells
Beyond modifying Cas proteins themselves, researchers can engineer the target cells to evade immune detection. A recent breakthrough demonstrated that CRISPR-Cas12b can create "hypoimmune" cells that avoid rejection without systemic immunosuppression [82]. This approach involves simultaneous knockout of HLA class I and II molecules (to protect against adaptive T-cell rejection) and overexpression of CD47 (to inhibit innate immune cell killing through macrophage and NK cell inhibition) [82].
Application Note: In a first-in-human study, CRISPR-edited hypoimmune pancreatic islet cells were transplanted into a patient with type 1 diabetes. The cells successfully engrafted and maintained stable function for 12 weeks without immunosuppressive drugs, demonstrating the potential of this approach to overcome immune rejection barriers [82].
Addressing preexisting immunity to Cas proteins requires a multi-faceted approach combining protein engineering, delivery optimization, and strategic immunosuppression. The field is rapidly advancing with solutions including epitope-modified Cas variants, AI-designed novel editors, and hypoimmune cell engineering. As CRISPR-based therapies progress toward broader clinical application, comprehensive immune risk assessment and mitigation must be integrated throughout the therapeutic development process. The protocols and strategies outlined here provide a framework for researchers to systematically evaluate and overcome immunological barriers in therapeutic cell design.
Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) and CRISPR-associated (Cas) systems have revolutionized the field of genetic engineering, offering unprecedented opportunities for therapeutic applications by permanently correcting deleterious base mutations or disrupting disease-causing genes with great precision and efficiency [37] [83]. The simplicity of the CRISPR-Cas9 system, which relies on a Cas nuclease and a guide RNA (gRNA) to create targeted double-strand breaks (DSBs) in the genome, has made it the most widely used genome editing technology in molecular biology laboratories worldwide [83] [84].
However, a fundamental roadblock in therapeutic genome editing is our inability to control how DNA perturbations are repaired [18]. The editing outcome is ultimately determined by how the cellular DNA repair machinery responds to the CRISPR-induced perturbation [18] [37]. This challenge is particularly pronounced in nondividing cells such as neurons and cardiomyocytes, which constitute the majority of cells in many clinically relevant tissues [18]. Surprisingly little is known about DNA repair in these postmitotic cells, which cannot regenerate yet must withstand an entire lifetime's worth of DNA damage [18].
This application note examines the unique DNA repair characteristics of neurons and cardiomyocytes, provides quantitative comparisons with dividing cells, details experimental methodologies for studying and manipulating repair outcomes, and discusses the implications for therapeutic genome editing in cardiovascular and neurological diseases.
Extended Repair Time Course in Postmitotic Cells
DNA repair kinetics differ dramatically between dividing and nondividing cells. In dividing cells such induced pluripotent stem cells (iPSCs), the repair half-life of Cas9-induced DSBs is typically between 1 and 10 hours, with indels plateauing within a few days [18]. In stark contrast, indels in neurons continue to increase for up to 2 weeks post-transduction [18] [85].
Table 1: Time Course of Indel Accumulation After CRISPR Editing
| Cell Type | Proliferation Status | Time to Peak Indel Formation | Key Observations |
|---|---|---|---|
| iPSCs | Dividing | Few days | Editing outcomes plateau rapidly |
| iPSC-derived neurons | Postmitotic | 16+ days | Continued increase in indels for over two weeks |
| iPSC-derived cardiomyocytes | Postmitotic | Similar extended timeline | Prolonged accumulation observed |
| Primary T cells (activated) | Dividing | Rapid resolution | DSBs resolved quickly to avoid cell cycle arrest |
| Primary T cells (resting) | Nondividing | Extended timeline | Similar to neurons despite different delivery method |
This prolonged timeline cannot be attributed solely to delivery deficits, as base editing in neurons was comparably efficient to iPSCs—and sometimes even more efficient—within only three days post-transduction [18]. The extended time course appears partially attributable to long-lived Cas9 protein, which remains active for over 30 days in neurons, enabling multiple cycles of cutting and repair [85].
Distinct DNA Repair Pathway Utilization
Postmitotic cells exhibit markedly different preferences for DNA repair pathways compared to their dividing counterparts. While dividing cells utilize both nonhomologous end joining (NHEJ) and microhomology-mediated end joining (MMEJ) pathways, neurons predominantly employ NHEJ, resulting in a narrower distribution of editing outcomes [18] [85].
Table 2: DNA Repair Pathway Preferences in Different Cell Types
| Repair Pathway | iPSCs (Dividing) | Neurons (Postmitotic) | Cardiomyocytes (Postmitotic) |
|---|---|---|---|
| NHEJ | Moderate usage | Predominant pathway | Expected to be predominant |
| MMEJ | Frequent usage | Limited usage | Expected to be limited |
| HDR | Available in cell cycle phases | Restricted (cell cycle dependent) | Restricted (cell cycle dependent) |
| Characteristic Outcome | Broad range of indels, larger deletions | Narrow distribution, smaller indels | Similar to neurons |
For every sgRNA tested, the ratio of insertions to deletions was significantly higher in neurons than iPSCs [18]. This pathway preference stems from the fundamental biological difference that postmitotic cells do not face replication checkpoints and thus might not be subjected to the same pressures to resolve DSBs mutagenically [18].
Molecular Mechanisms Underlying Cell-Type Specific Repair
The differential repair outcomes in neurons versus dividing cells are mediated by distinct molecular responses to DNA damage. Transcriptomic profiling reveals that neurons mount a unique gene expression response to CRISPR-induced damage, upregulating DNA repair and replication-associated genes, including non-canonical activation of RRM2, a ribonucleotide reductase subunit [85].
This unique repair signature in neurons represents a potentially tunable system. Pharmacological or siRNA-mediated inhibition of RRM2 and associated repair factors has been shown to shift editing outcomes by increasing deletions and overall indel efficiency [85]. The diagram below illustrates the differential DNA repair mechanisms in dividing versus nondividing cells.
Experimental Protocols for Studying and Manipulating DNA Repair
Protocol: Efficient Delivery of CRISPR Components to Neurons
Traditional transfection methods are inefficient for postmitotic neurons. Virus-like particles (VLPs) provide an effective alternative for delivering CRISPR machinery to these challenging cells [18].
Materials:
- Human iPSC-derived neurons (≥95% NeuN-positive)
- VSVG-pseudotyped HIV VLPs or VSVG/BRL-co-pseudotyped FMLV VLPs
- Cas9 ribonucleoprotein (RNP) complex
- Appropriate neuronal culture media
Procedure:
- Differentiate iPSCs to cortical-like excitatory neurons using established protocols [18]. Confirm postmitotic status by Ki67 immunocytochemistry (should be >99% negative by Day 7) and neuronal purity by NeuN staining (should be ~95% positive from Day 4 onward).
- Produce VLPs containing Cas9 RNP using preferred pseudotyping approach. VSVG pseudotyping targets LDLR-expressing cells including neurons, while BaEVRless (BRL) co-pseudotyping improves transduction in multiple human cell types [18].
- Transduce neurons with VLPs at appropriate multiplicity of infection. Monitor transduction efficiency using co-delivered fluorescent markers like mNeonGreen.
- Confirm DSB formation via immunocytochemistry for γH2AX and 53BP1 colocalization at 24-48 hours post-transduction.
- Harvest cells at multiple time points (from 3 days to 16 days post-transduction) to track the extended time course of indel accumulation.
Validation: Editing efficiency can reach up to 97% with optimized VLP delivery [18]. Confirm DSB resolution and editing outcomes by tracking γH2AX foci disappearance and performing indel analysis via next-generation sequencing.
Protocol: Modulating DNA Repair Outcomes in Nondividing Cells
The unique DNA repair environment in neurons provides opportunities to direct editing outcomes through chemical or genetic perturbations [18] [85].
Materials:
- RRM2 inhibitors (e.g., hydroxyurea) or siRNA targeting RRM2
- All-in-one lipid nanoparticles for co-delivery of Cas9, sgRNA, and siRNAs
- Appropriate controls (scrambled siRNA, DMSO vehicle)
Procedure:
- Design sgRNAs considering that neurons exhibit different repair outcomes than dividing cells even with identical sgRNAs [18]. Use established tools (CHOPCHOP, CRISPR Design Tool) for sgRNA design [86].
- Select target genes for perturbation based on transcriptomic data. RRM2 is a key target identified in neuronal repair responses [85].
- Deliver CRISPR components and repair modulators simultaneously using all-in-one lipid nanoparticles that co-encapsulate Cas9 RNP and siRNA targeting repair factors [85].
- Assess editing outcomes by tracking indel spectra over an extended time course (up to 16 days). NHEJ-dominated repair in neurons typically produces smaller indels compared to dividing cells.
- Quantify efficiency shifts by comparing perturbation conditions to controls. Successful modulation should increase deletion frequency and overall indel efficiency.
Applications: This approach has been successfully applied to direct DNA repair toward desired editing outcomes in nondividing human neurons, cardiomyocytes, and primary T cells [18].
The experimental workflow for studying cell-type specific repair encompasses both delivery and modulation strategies, as shown in the diagram below.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Studying Cell-Type Specific DNA Repair
| Reagent/Category | Specific Examples | Function/Application | Considerations for Postmitotic Cells |
|---|---|---|---|
| Delivery Systems | VSVG-pseudotyped HIV VLPs, VSVG/BRL-co-pseudotyped FMLV VLPs | Efficient Cas9 RNP delivery to neurons | Up to 97% transduction efficiency; VSVG targets LDLR [18] |
| CRISPR Components | Synthetic sgRNA, Cas9 RNPs | Genome editing with reduced off-target effects | Synthetic sgRNA offers high purity; chemical synthesis enables modifications [87] |
| Cell Models | iPSC-derived neurons, iPSC-derived cardiomyocytes | Physiologically relevant human models | Confirm postmitotic status (Ki67-negative, NeuN-positive) [18] |
| Repair Modulators | RRM2 inhibitors, siRNA pools | Direct DNA repair pathway choice | Lipid nanoparticles enable co-delivery with CRISPR components [85] |
| Analysis Tools | NGS for indel spectra, γH2AX/53BP1 immunofluorescence | Assess editing outcomes and DSB resolution | Track outcomes over extended timelines (weeks, not days) [18] |
The unique DNA repair characteristics of neurons and cardiomyocytes present both challenges and opportunities for therapeutic genome editing. The extended repair timeline and distinct pathway preferences in these postmitotic cells necessitate a fundamental rethinking of editing strategies developed in dividing cells [18].
The ability to manipulate the DNA repair response in nondividing cells with chemical or genetic perturbations provides a promising avenue for enhancing therapeutic editing precision and efficiency [18] [85]. By targeting specific repair factors like RRM2 that are uniquely upregulated in neurons, researchers can shift editing outcomes toward desired patterns.
These findings have profound implications for treating genetically driven cardiovascular diseases and neurological disorders [18] [88]. As CRISPR-Cas9 technology continues to evolve, with developments including base editors, prime editors, and epigenetic modifiers, understanding cell-type specific repair mechanisms will be essential for harnessing the full therapeutic potential of genome editing in clinically relevant tissues [37] [89].
The translation of CRISPR-Cas genome editing from a powerful research tool to clinically approved therapies presents a complex landscape of manufacturing and regulatory challenges. The journey from discovery to clinical delivery requires meticulous planning, stringent quality control, and adherence to evolving regulatory frameworks. Central to this process is the production of Good Manufacturing Practice (GMP)-grade reagents and the design of robust clinical pathways that ensure both efficacy and patient safety [90] [30]. This application note provides a structured overview of GMP production requirements, regulatory considerations, and essential experimental protocols for researchers and drug development professionals advancing CRISPR-based therapeutic cell designs.
GMP Manufacturing: sgRNA Grades and Quality Control
Spectrum of sgRNA Products for Therapeutic Development
The quality of single guide RNA (sgRNA) is a critical determinant of successful CRISPR gene editing. Suppliers provide different grades of sgRNA tailored to specific stages of the therapeutic development pipeline, with varying levels of documentation, quality control, and regulatory compliance [90] [91].
Table 1: sgRNA Grades for CRISPR Therapeutic Development
| sgRNA Grade | Intended Use | Manufacturing Environment | Quality Documentation | Key Applications |
|---|---|---|---|---|
| Research Use Only (RUO) | Discovery and proof-of-concept studies | ISO 9001:2015 conditions | Limited | Functional genomics, target validation, early-stage research [90] [91] |
| INDe/Engineering Run | IND-enabling research, toxicity studies | Controlled environment, equivalent to GMP processes | Draft batch records, limited QA oversight | Preclinical safety studies, bridging research and clinical development [90] [91] |
| cGMP | Clinical trials and human therapeutic use | ICH Q7 compliant facility, ISO 8 Clean Room | Full QA oversight, comprehensive release testing | Clinical applications requiring regulatory compliance for human use [90] [91] [92] |
Essential Quality Control Testing for GMP sgRNA
Comprehensive quality control is fundamental for GMP-grade sgRNAs intended for clinical applications. The following tests are critical for ensuring product safety, identity, purity, and potency.
Table 2: Essential Quality Control Tests for GMP sgRNA
| Category | Attribute | Testing Method | Purpose |
|---|---|---|---|
| Identity | Molecular weight | ESI-MS | Confirms correct molecular composition [91] |
| Sequence verification | NGS-based gRNA sequencing | Validates full-length sequence identity and detects contaminants [91] | |
| Purity | Purity analysis | Single-channel CE or LC-MS | Quantifies sgRNA purity and process-related impurities [91] |
| Elemental impurities | USP <233> | Detaces residual metal contaminants [91] | |
| Residual solvents | USP <467> | Identifies and quantifies harmful solvent residues [91] | |
| Safety | Endotoxin testing | USP <85> limulus amebocyte lysate (LAL) | Ensures products are free from pyrogenic contaminants [91] |
| Bioburden testing | USP <61/62> | Confirms sterility and absence of microbial contamination [91] | |
| Yield | Concentration | UV/Vis Optical density at 260nm | Quantifies final product yield [91] |
| General | Appearance | Visual inspection | Assesses physical characteristics [91] |
Regulatory Pathway Design for CRISPR Therapeutics
FDA Regulatory Framework for Genome Editing Products
The regulatory landscape for CRISPR-based therapies is complex and continuously evolving. The U.S. Food and Drug Administration (FDA) has issued specific guidance documents to address the unique challenges presented by gene editing products [93].
Key FDA guidances relevant to CRISPR therapeutics include:
- Human Gene Therapy Products Incorporating Human Genome Editing (January 2024) [93]
- Chemistry, Manufacturing, and Control (CMC) Information for Human Gene Therapy Investigational New Drug Applications (INDs) (January 2020) [93]
- Long Term Follow-up After Administration of Human Gene Therapy Products (January 2020) [93]
- Considerations for the Development of Chimeric Antigen Receptor (CAR) T Cell Products (January 2024) [93]
Regulatory agencies require comprehensive assessment of both on-target and off-target effects as well as evaluation of structural genomic integrity to ensure the safety of therapeutic gene editing applications [62].
Regulatory Pathway for CRISPR Therapeutics: This diagram illustrates the progressive stages of therapeutic development, aligned with appropriate sgRNA grades and major regulatory milestones from discovery to approval.
Risk Mitigation and Safety Assessment Strategies
Beyond standard regulatory requirements, CRISPR therapeutics require specific safety assessments to address unique risks associated with genome editing, particularly structural variations and off-target effects [62].
Comprehensive Safety Assessment Protocol:
- On-Target Genomic Aberration Analysis: Employ long-read sequencing technologies (e.g., PacBio, Oxford Nanopore) to detect large-scale deletions, chromosomal rearrangements, and complex structural variations that may be missed by short-read sequencing [62].
- Off-Target Effect Assessment: Utilize genome-wide methods such as CAST-Seq and LAM-HTGTS to identify chromosomal translocations and off-target activity across the genome [62].
- Tumorigenicity Risk Evaluation: Implement in vitro and in vivo models to assess potential oncogenic transformation resulting from unintended edits in tumor suppressor genes or proto-oncogenes [62].
- Immunogenicity Profiling: Characterize cellular immune responses to CRISPR components, including pre-existing immunity to bacterial Cas proteins [45].
Experimental Protocols for Safety and Efficacy Assessment
Protocol: Comprehensive Off-Target Assessment Using CAST-Seq
Objective: To identify and quantify CRISPR-Cas9-induced structural variations and chromosomal translocations genome-wide.
Materials:
- Cells edited with CRISPR-Cas9 complex
- CAST-Seq kit or components: biotinylated adapters, PCR reagents, NGS library preparation kit
- Next-generation sequencing platform
- Bioinformatics pipeline for CAST-Seq analysis
Methodology:
- Cell Preparation and Editing:
- Transfect or electroporate target cells with CRISPR-Cas9 ribonucleoprotein (RNP) complex containing your specific sgRNA.
- Include appropriate controls (non-edited cells, mock-transfected cells).
- Culture cells for 72 hours post-editing to allow expression of potential structural variations.
DNA Extraction and Quality Control:
- Extract genomic DNA using high-molecular-weight DNA extraction kit.
- Quantify DNA concentration and assess integrity by agarose gel electrophoresis.
CAST-Seq Library Preparation:
- Digest genomic DNA with frequently cutting restriction enzymes (4bp cutters).
- Ligate biotinylated adapters to digested DNA fragments.
- Perform two consecutive PCR rounds with specific primers targeting the on-site and potential off-site regions.
- Purify PCR products and prepare NGS libraries following manufacturer's instructions.
Sequencing and Data Analysis:
- Sequence libraries on appropriate NGS platform (minimum recommended coverage: 10 million reads per sample).
- Analyze data using CAST-Seq bioinformatics pipeline to identify:
- On-target editing efficiency
- Off-target sites with sequence similarity to the target site
- Chromosomal translocations and large structural variations
Interpretation and Reporting:
- Quantify frequency of identified off-target events and structural variations.
- Annotate affected genomic regions (e.g., coding sequences, regulatory elements).
- Assess potential functional impact of identified variations [62].
Protocol: GMP-Grade sgRNA Quality Control Testing
Objective: To perform comprehensive quality control testing of GMP-grade sgRNA to ensure compliance with regulatory standards.
Materials:
- GMP-grade sgRNA sample
- Electrospray ionization mass spectrometry (ESI-MS) system
- Next-generation sequencing platform
- Capillary electrophoresis (CE) or liquid chromatography-mass spectrometry (LC-MS) system
- Endotoxin testing kit (LAL assay)
- Bioburden testing materials
- UV/Vis spectrophotometer
Methodology:
- Identity Testing:
- Molecular Weight Confirmation:
- Prepare sgRNA sample at appropriate concentration for ESI-MS.
- Perform ESI-MS analysis and compare observed molecular weight to theoretical value.
- Acceptance criterion: ± 50 Da of theoretical molecular weight.
- Sequence Verification:
- Prepare sequencing library using NGS-based gRNA sequencing protocol.
- Sequence with minimum 500x read depth across the spacer region.
- Analyze data for sequence identity and potential contaminants.
- Acceptance criterion: >95% sequence identity to reference [91].
- Molecular Weight Confirmation:
Purity Analysis:
- Purity Assessment:
- Perform CE or LC-MS analysis following manufacturer's protocols.
- Quantify full-length sgRNA and identify truncated impurities.
- Acceptance criterion: >90% full-length product.
- Elemental Impurities and Residual Solvents:
- Perform USP <233> and USP <467> testing as applicable.
- Ensure levels are below specified safety thresholds [91].
- Purity Assessment:
Safety Testing:
- Endotoxin Testing:
- Perform limulus amebocyte lysate (LAL) assay per USP <85>.
- Acceptance criterion: <0.5 EU/mg of sgRNA.
- Bioburden Testing:
- Perform USP <61/62> testing for microbial contamination.
- Acceptance criterion: No microbial growth observed [91].
- Endotoxin Testing:
Yield Determination:
- Measure optical density at 260nm using UV/Vis spectrophotometer.
- Calculate concentration and total yield [91].
CRISPR Safety Assessment Workflow: This diagram outlines the key steps in a comprehensive safety assessment protocol for CRISPR-edited therapeutic cells, highlighting critical methods for detecting structural variations and off-target effects.
The Scientist's Toolkit: Essential Research Reagent Solutions
Advancing CRISPR-based therapeutic cell designs requires access to specialized reagents and services that meet rigorous quality standards. The following toolkit summarizes key solutions for successful translation from research to clinic.
Table 3: Essential Research Reagent Solutions for CRISPR Therapeutic Development
| Reagent/Service | Function | Key Specifications | Application Notes |
|---|---|---|---|
| GMP sgRNA | Guides Cas nuclease to specific genomic target | >90% purity, full sequence verification, endotoxin-free | Required for clinical trials; ensures consistency and safety [90] [92] |
| GMP Cas Nuclease | Creates double-stranded breaks at target DNA site | High purity, validated activity, low endotoxin | Available as SpCas9 or engineered variants with enhanced specificity [92] |
| INDe sgRNA | Bridge between research and clinical-grade reagents | Controlled manufacturing, partial documentation | Ideal for IND-enabling studies and toxicology assessments [90] |
| gRNA Sequencing Service | Orthogonal identity confirmation | NGS-based, >500x read depth in spacer region | Critical for regulatory filings; detects sequence contaminants [91] |
| HPLC-Purified sgRNA | Enhanced purity for sensitive applications | >95% full-length product, reduced impurities | Improves editing efficiency in difficult-to-transfect cells [91] |
| Engineered Cas Variants | Increased specificity or altered PAM requirements | High-fidelity mutants, compact sizes for viral delivery | Reduces off-target effects; enables targeting of previously inaccessible sites [45] |
Successfully navigating the manufacturing and regulatory hurdles for CRISPR-based therapeutics requires a strategic approach that integrates GMP production planning with rigorous safety assessment from the earliest stages of development. Key success factors include: (1) early adoption of quality-controlled reagents that enable seamless transition from research to clinical stages; (2) implementation of comprehensive safety assessment protocols that detect both conventional off-target effects and large structural variations; and (3) proactive regulatory planning that addresses the unique challenges of genome editing products. By addressing these considerations throughout the development pipeline, researchers can accelerate the translation of CRISPR-based therapeutic cell designs from bench to bedside while maintaining the highest standards of safety and efficacy.
Within the framework of therapeutic cell design, achieving precise genomic modifications in postmitotic cells—such as neurons and cardiomyocytes—represents a significant challenge. Unlike proliferating cells, postmitotic cells have exited the cell cycle and consequently employ distinct DNA repair mechanisms, leading to different CRISPR-Cas9 editing outcomes [94]. The homologous directed repair (HDR) pathway, which requires cell cycle progression, is largely inaccessible in these cells, making them reliant on error-prone repair pathways like non-homologous end joining (NHEJ) [17]. This fundamental biological constraint directly impacts the efficiency and safety of CRISPR-based therapies for neurological and cardiac diseases. This Application Note provides a detailed experimental framework for characterizing and manipulating DNA repair in postmitotic cells to steer CRISPR-Cas9 editing outcomes toward precise, therapeutically relevant modifications.
DNA Repair Pathway Dynamics in Postmitotic Cells
Differential Repair in Dividing vs. Non-Dividing Cells
Recent comparative studies using isogenic induced pluripotent stem cells (iPSCs) and iPSC-derived neurons have revealed profound differences in how postmitotic cells process CRISPR-Cas9-induced double-strand breaks (DSBs). Neurons exhibit a markedly prolonged timeline for resolving DSBs, with insertion/deletion mutations (indels) continuing to accumulate for up to two weeks post-transduction, compared to just days in iPSCs [94]. This extended repair window in neurons suggests fundamentally different regulatory mechanisms for DNA damage response.
Table 1: Kinetic Comparison of DNA Repair in Dividing vs. Postmitotic Cells
| Repair Parameter | iPSCs (Dividing) | Neurons (Postmitotic) | Experimental Evidence |
|---|---|---|---|
| Time to indel plateau | 2-4 days | 14-16 days | Longitudinal sequencing [94] |
| Predominant repair pathways | MMEJ, NHEJ, HDR | Primarily NHEJ | Indel distribution analysis [94] |
| Ratio of insertions to deletions | Lower | Significantly higher | Multiple sgRNA testing [94] |
| Large deletion frequency | Context-dependent | Potentially elevated with NHEJ inhibition | Amplicon sequencing [62] |
| HDR efficiency | Moderate | Very low | Donor template incorporation [17] |
The repair outcome distribution also differs substantially. While iPSCs display a broad range of indels with a prevalence of larger deletions typically associated with microhomology-mediated end joining (MMEJ), neurons predominantly produce smaller indels characteristic of classical NHEJ (cNHEJ) [94]. This pathway preference has direct implications for therapeutic editing strategies, as it inherently limits the repertoire of achievable mutations in postmitotic cells.
DNA Repair Pathway Diagram
The following diagram illustrates the competing DNA repair pathways active in postmitotic cells following CRISPR-Cas9-induced DSBs, highlighting potential intervention points for manipulating outcomes.
Experimental Protocols for Editing Outcome Control
Characterizing Editing Outcomes in Postmitotic Cells
Protocol: Longitudinal Analysis of Indel Accumulation
Purpose: To quantitatively track the kinetics of CRISPR-Cas9 editing outcomes in postmitotic cells over time.
Materials:
- iPSC-derived postmitotic cells (neurons or cardiomyocytes)
- CRISPR-Cas9 components delivered via virus-like particles (VLPs)
- Tissue culture reagents and equipment
- Genomic DNA extraction kit
- Barcoded deep sequencing platform
Procedure:
- Differentiate iPSCs into postmitotic neurons using established protocols [94]. Validate postmitotic status via immunocytochemistry for Ki67 (≤1% positive) and neuronal markers (≥95% NeuN positive by Day 7).
- Deliver CRISPR-Cas9 using VSVG-pseudotyped HIV VLPs or VSVG/BRL-co-pseudotyped FMLV VLPs [94]. Standardize Cas9 RNP doses between experimental groups.
- Harvest genomic DNA at multiple time points: days 1, 2, 4, 7, 14, and 21 post-transduction using a silica membrane-based extraction method.
- Amplify target loci using barcoded primers with Illumina adapter sequences. Pool amplicons for high-throughput sequencing.
- Analyze sequencing data using computational pipelines (e.g., CRISPResso2) to quantify indel percentages, size distributions, and sequences at each time point.
Expected Results: Indel percentages in postmitotic cells will increase gradually, reaching plateau only after 14-16 days, in contrast to the rapid plateau within 2-4 days observed in iPSCs [94].
Strategic Manipulation of DNA Repair Pathways
Chemical and Genetic Interventions
Multiple strategies exist to modulate the DNA repair environment in postmitotic cells. The table below summarizes key approaches, their mechanisms, and outcomes.
Table 2: DNA Repair Modulation Strategies for Postmitotic Cells
| Intervention Category | Example Reagents/Tools | Mechanism of Action | Effect on Editing Outcomes | Considerations & Risks |
|---|---|---|---|---|
| NHEJ inhibition | DNA-PKcs inhibitors (AZD7648) | Blocks key NHEJ pathway kinase | Increases large deletions & chromosomal aberrations [62] | High risk of structural variations; use with caution |
| MMEJ modulation | POLQ inhibition | Suppresses polymerase theta-mediated MMEJ | Reduces kb-scale deletions when combined with DNA-PKcs inhibition [62] | Does not prevent Mb-scale deletions |
| HDR enhancement | 53BP1 inhibition | Removes barrier to end resection | May increase HDR without elevating translocation frequency [62] | Limited effect in postmitotic cells due to cell cycle dependence |
| p53 pathway modulation | Pifithrin-α | Transient p53 inhibition | Reduces large chromosomal aberrations [62] | Oncogenic concerns with prolonged suppression |
| Alternative NHEJ suppression | Combined DNA-PKcs and POLQ inhibition | Dual blockade of NHEJ and MMEJ | Protective against kb-scale deletions [62] | Complex pathway interactions |
Protocol: DNA Repair Modulation for Precise Editing
Purpose: To enhance precise editing outcomes in postmitotic cells through pharmacological manipulation of DNA repair pathways.
Materials:
- iPSC-derived neurons (14-21 days post-differentiation)
- CRISPR-Cas9 RNP complexes with donor template
- DNA repair modulators (e.g., small molecule inhibitors)
- VLP or nucleofection delivery system
- Genomic DNA extraction and analysis reagents
Procedure:
- Prepare donor template using the SMART (Silently Mutate And Repair Template) design strategy [95]. Incorporate silent mutations in the gap sequence between Cas9 cut and insertion sites to prevent base pairing with target DNA while maintaining amino acid coding.
- Pre-treat neurons with selected DNA repair modulators for 6-24 hours prior to CRISPR delivery. For example, use pifithrin-α (10-20 µM) to transiently inhibit p53 signaling.
- Deliver CRISPR-Cas9 components as RNP complexes via VLPs or nucleofection. For SMART-based editing, co-deliver Cas9 RNP with SMART donor template.
- Maintain modulator treatment for 48-72 hours post-editing, then replace with standard culture medium.
- Assess editing outcomes at day 21 post-editing using long-range PCR and sequencing to detect both precise edits and structural variations.
Expected Results: SMART template design can significantly improve knock-in efficiency at distances >40 bp from the cut site [95]. Combined with appropriate DNA repair modulation, precise editing efficiency can be enhanced while minimizing on-target structural variations.
Advanced Genome Editing Workflow
The following diagram outlines a comprehensive experimental workflow for controlling editing outcomes in postmitotic cells, integrating the key protocols and strategies described above.
Research Reagent Solutions
Table 3: Essential Reagents for DNA Repair Manipulation Studies
| Reagent Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| Delivery Systems | VSVG/BRL-pseudotyped FMLV VLPs [94] | Efficient RNP delivery to postmitotic cells | Up to 97% transduction efficiency in human neurons |
| CRISPR Formats | Pre-complexed RNP complexes [95] | Direct delivery of active editing machinery | Faster editing, reduced off-target effects |
| Template Design | SMART donor templates [95] | Enhanced HDR efficiency regardless of PAM position | Maintains amino acid sequence with silent mutations |
| NHEJ Inhibitors | DNA-PKcs inhibitors (AZD7648) [62] | Suppresses classical NHEJ pathway | Risk of large structural variations |
| Pathway Modulators | Pifithrin-α [62] | Transient p53 inhibition | Reduces chromosomal aberrations |
| Validation Tools | Barcoded deep sequencing [94] | Quantitative tracking of editing outcomes | Detects both indels and structural variations |
| Cell Systems | iPSC-derived neurons [94] | Physiologically relevant postmitotic model | Genetically identical to iPSC controls for comparative studies |
The unique DNA repair environment of postmitotic cells necessitates specialized approaches for controlling CRISPR-Cas9 editing outcomes. The extended timeline of indel accumulation and predominant use of NHEJ pathways in these cells present both challenges and opportunities for therapeutic genome editing. By employing the characterization and modulation strategies outlined in this Application Note—including longitudinal kinetic analysis, SMART template design, and selective pathway manipulation—researchers can significantly enhance the precision and safety of genomic modifications in postmitotic cells. These advances are crucial for developing effective CRISPR-based therapies for neurological and cardiac disorders, where precise editing of non-dividing cells is paramount. Continued refinement of these approaches will further bridge the gap between in vitro editing efficiency and clinically viable therapeutic outcomes.
Analytical Frameworks: Validating Editing Efficacy and Comparing Gene Editing Platforms
Within the field of therapeutic cell design, the precise validation of CRISPR-Cas genome editing outcomes is a critical step in developing safe and effective treatments. Accurate measurement of editing efficiency, specificity, and the resulting spectrum of mutations is essential for translating laboratory research into clinical applications [4]. This application note provides a detailed comparison of four key validation methodologies—Next-Generation Sequencing (NGS), T7 Endonuclease I (T7E1) assay, Tracking of Indels by Decomposition (TIDE), and Indel Detection by Amplicon Analysis (IDAA)—framed within the context of therapeutic cell engineering. We present structured comparative data, detailed experimental protocols, and workflow visualizations to guide researchers in selecting and implementing the most appropriate validation strategy for their specific therapeutic development goals.
Comparative Analysis of CRISPR Validation Methods
The selection of a validation method involves balancing factors such as quantitative accuracy, informational depth, throughput, cost, and technical feasibility. The table below provides a systematic comparison of these critical parameters for the four methodologies.
Table 1: Comprehensive Comparison of CRISPR-Cas Genome Editing Validation Methodologies
| Method | Detection Principle | Quantitative Capability | Information Depth | Throughput | Approximate Cost | Primary Therapeutic Application |
|---|---|---|---|---|---|---|
| NGS | High-throughput sequencing of PCR amplicons [96] | High (Absolute quantification) [97] | High (Full spectrum of indels, complex events) [96] [97] | High (Once established) | High | Clinical-grade validation, off-target assessment, characterizing complex editing outcomes [4] |
| T7E1 Assay | Mismatch cleavage of heteroduplex DNA [96] [98] | Semi-quantitative (Underestimates complex indels) [98] [99] | Low (Only indicates presence of indels) [96] | Medium | Low | Rapid, low-cost preliminary screening during gRNA and protocol optimization [96] |
| TIDE | Decomposition of Sanger sequencing chromatograms [96] [98] | Medium (Computational inference of efficiency) [99] | Medium (Indel frequency and predominant types) [96] | Medium | Low-Medium | Intermediate analysis for research-stage cell lines where NGS is impractical [96] |
| IDAA | Capillary electrophoresis of fluorescently labelled amplicons [99] | Medium (Based on fragment size) [99] | Medium (Indel size distribution, no sequence data) [99] | High | Medium | High-throughput screening of gRNA efficiency and clonal populations [99] |
Detailed Experimental Protocols
Next-Generation Sequencing (NGS) for Comprehensive Editing Analysis
NGS is considered the gold standard for CRISPR validation, providing a comprehensive, quantitative, and unbiased view of editing outcomes, which is crucial for preclinical safety assessment [96] [97].
Procedure:
- Genomic DNA Extraction: Extract high-quality genomic DNA from edited and control cell populations using a standard silica-column or magnetic-bead based method. Ensure accurate quantification, for example via fluorometry.
- Primary PCR Amplification: Design primers flanking the target site to generate an amplicon of optimal length for your sequencing platform (typically 300-500 bp). Use a high-fidelity DNA polymerase to minimize PCR-introduced errors. The number of PCR cycles should be kept as low as possible to avoid skewing allele frequencies.
- Library Preparation and Barcoding: Purify the primary PCR product. In a second, limited-cycle PCR, add platform-specific adapters and unique dual indices (barcodes) to each sample to allow for multiplexing.
- Sequencing: Pool the barcoded libraries at equimolar concentrations and sequence on an Illumina MiSeq, NovaSeq, or comparable platform to achieve high coverage (typically >50,000x read depth per sample).
- Bioinformatic Analysis: Process the raw sequencing data through a pipeline such as CRISPResso2 [97] to align reads to a reference sequence and quantify the percentage and types of indels and other modifications.
T7 Endonuclease I (T7E1) Mismatch Cleavage Assay
The T7E1 assay is a rapid, non-sequencing based method to detect the presence of induced mutations but lacks quantitative precision and sequence-level information [96] [98].
Procedure:
- PCR Amplification: Amplify the target region from edited and control genomic DNA using standard Taq polymerase.
- Heteroduplex Formation: Purify the PCR product. To form heteroduplexes between wild-type and edited DNA strands, denature the PCR product at 95°C for 5-10 minutes and then slowly reanneal by ramping the temperature down to 25°C at a rate of 0.1°C per second in a thermal cycler.
- T7E1 Digestion: Treat the heteroduplexed DNA with T7 Endonuclease I, which cleaves at mismatched sites. Use 200-400 ng of purified PCR product, 1 µL of T7E1 enzyme (M0302, New England Biolabs) in 1X NEBuffer 2 in a total volume of 10-20 µL. Incubate at 37°C for 30-60 minutes [98].
- Analysis by Gel Electrophoresis: Resolve the digestion products on a 2-3% agarose gel. Cleavage products will appear as lower molecular weight bands. Editing efficiency can be estimated semi-quantitatively using densitometry software with the formula: % Indel = (1 - √(1 - (b+c)/(a+b+c))) × 100, where
ais the integrated intensity of the undigested PCR product band, andbandcare the intensities of the cleavage products [98].
Tracking of Indels by Decomposition (TIDE)
TIDE provides a quantitative breakdown of indel frequencies from Sanger sequencing data, offering a cost-effective balance between information and throughput [96] [99].
Procedure:
- Sample Preparation and Sequencing: PCR-amplify the target locus from both edited and control (wild-type) samples. Purify the PCR products and submit them for Sanger sequencing using one of the PCR primers.
- Data Upload: Access the TIDE web tool (http://shinyapps.datacurators.nl/tide/). Upload the Sanger sequencing chromatogram files (in
.ab1format) for both the wild-type control and the edited sample. - Parameter Configuration: Input the gRNA target sequence and identify the expected cut site (typically 3-4 bp upstream of the PAM sequence). Set the indel size range for analysis (e.g., -20 to +10 bp) and define the sequence decomposition window, ensuring it encompasses the edited region [98] [99].
- Analysis and Interpretation: The TIDE algorithm will decompose the mixed sequencing trace from the edited sample and report the overall editing efficiency (% indels), the size and frequency of individual indel events, and a statistical goodness-of-fit (R²) for the decomposition.
Indel Detection by Amplicon Analysis (IDAA)
IDAA combines PCR amplification with fluorescent labeling and capillary electrophoresis to determine indel size distributions in a high-throughput manner, though it does not provide sequence information [99].
Procedure:
- Fluorescent PCR Amplification: Perform a PCR amplification of the target locus using a 5'-fluorescently labelled (e.g., 6-FAM) forward primer and a standard reverse primer.
- Fragment Analysis: Dilute the fluorescently labelled PCR product and mix it with a size standard. Denature the samples and run them on a capillary electrophoresis instrument (e.g., ABI 3500 Genetic Analyzer).
- Data Analysis: The instrument software will generate an electrophoretogram with peaks corresponding to different PCR fragment lengths. The distribution of peak sizes and their fluorescent intensities directly correspond to the variety and frequency of indels in the sample population.
The Scientist's Toolkit: Essential Research Reagents
The successful implementation of the above protocols relies on a suite of key reagents and tools. The following table details these essential components.
Table 2: Key Research Reagent Solutions for CRISPR Validation
| Reagent / Tool | Function | Example Product / Specification |
|---|---|---|
| High-Fidelity DNA Polymerase | Accurate amplification of the target locus for NGS and cloning. | Q5 Hot Start High-Fidelity 2X Master Mix (M0494, NEB) [98] |
| T7 Endonuclease I | Enzyme for mismatch cleavage in the T7E1 assay. | T7 Endonuclease I (M0302, New England Biolabs) [98] |
| cGMP Guide RNA | Clinically relevant, high-quality guide RNA for therapeutic development. | GenScript's scalable cGMP guide RNA production [100] |
| NGS Library Prep Kit | Preparation of sequencing-ready libraries from PCR amplicons. | Illumina DNA Prep Kit |
| ICE Analysis Software | User-friendly webtool for analyzing Sanger sequencing data to determine editing efficiency and indel distribution. | Synthego's Inference of CRISPR Edits (ICE) [96] |
| CRISPResso2 Software | Bioinformatics tool for detailed analysis of NGS data from genome editing experiments. | Open-source software for quantifying editing outcomes [97] |
Workflow and Relationship Visualizations
The following diagrams illustrate the logical workflows and key relationships for the discussed CRISPR validation methodologies.
CRISPR Validation Method Selection
Core NGS Workflow for Editing Analysis
T7E1 Assay Procedure
DNA Repair Pathways Activated by CRISPR-Cas9
The advent of programmable gene editing technologies has revolutionized therapeutic cell design, offering researchers unprecedented precision in genomic manipulation. Among these technologies, Zinc Finger Nucleases (ZFNs), Transcription Activator-Like Effector Nucleases (TALENs), and Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR-Cas9) represent three generations of engineered nucleases that facilitate targeted DNA double-strand breaks (DSBs) [101] [54]. These platforms operate through a shared fundamental mechanism: inducing site-specific DSBs in the genome, which subsequently activate endogenous cellular repair pathways—primarily non-homologous end joining (NHEJ) or homology-directed repair (HDR) [101] [45]. The choice between these platforms significantly impacts the efficiency, specificity, and ultimate success of therapeutic applications, from ex vivo cell engineering to in vivo gene therapies. This application note provides a detailed comparative analysis of these technologies, emphasizing their performance metrics in therapeutic contexts and providing standardized protocols for their implementation in research settings.
Technology Comparison and Performance Metrics
Mechanism of Action and Design
Each editing platform employs a distinct molecular architecture for DNA recognition and cleavage [101] [54]:
ZFNs are fusion proteins comprising an array of engineered zinc finger domains (each recognizing 3-4 bp) fused to the FokI nuclease domain. ZFNs function as pairs, binding opposing DNA strands with a spacer sequence between them. FokI dimerization is required for DNA cleavage, which generates DSBs with 5' overhangs [101].
TALENs similarly utilize the FokI nuclease domain but employ TALE (Transcription Activator-Like Effector) repeat arrays for DNA recognition. Each TALE repeat, consisting of 33-35 amino acids, recognizes a single nucleotide through Repeat-Variable Diresidues (RVDs), with specific RVD codes (NG for T, NI for A, HD for C, and NN/HN/NK for G) [101] [54]. Like ZFNs, TALENs operate as pairs requiring dimerization for activity.
CRISPR-Cas9 employs a fundamentally different mechanism based on RNA-DNA recognition. The system consists of two key components: the Cas9 nuclease and a guide RNA (gRNA). The gRNA, a synthetic fusion of crRNA and tracrRNA, directs Cas9 to complementary genomic loci adjacent to a Protospacer Adjacent Motif (PAM) sequence (5'-NGG-3' for Streptococcus pyogenes Cas9) [45]. Cas9 then generates blunt-ended DSBs at the target site.
Table 1: Fundamental Characteristics of Gene Editing Platforms
| Feature | ZFNs | TALENs | CRISPR-Cas9 |
|---|---|---|---|
| DNA Recognition Mechanism | Protein-DNA (Zinc finger domains) | Protein-DNA (TALE repeats) | RNA-DNA (gRNA complementarity) |
| Nuclease Domain | FokI | FokI | Cas9 |
| Recognition Site Length | 9-18 bp (per monomer) | 14-20 bp (per monomer) | 20 nt + PAM (gRNA) |
| Dimerization Required | Yes | Yes | No |
| Target Design Constraints | Target sites every 50-200 bp in random DNA | Must begin with T; flexible site selection | Requires PAM sequence (5'-NGG-3' for SpCas9) |
| Repair Pathways Engaged | NHEJ, HDR | NHEJ, HDR | NHEJ, HDR |
Performance Metrics and Clinical Relevance
Recent comparative studies and clinical trial data reveal significant differences in efficiency, specificity, and practical implementation across platforms [102] [54] [103]:
Editing Efficiency: CRISPR-Cas9 generally demonstrates superior editing efficiency across multiple cell types. A comparative study targeting human papillomavirus (HPV) genes found SpCas9 to be more efficient than both ZFNs and TALENs [103]. CRISPR's efficiency stems from its simplified design, where only the gRNA sequence needs modification for new targets.
Specificity and Off-Target Effects: Off-target activity remains a critical consideration for therapeutic applications. GUIDE-seq analysis revealed that ZFNs can generate substantial off-target events (287-1,856 in HPV studies), with specificity potentially correlating with middle "G" counts in zinc finger proteins [103]. TALENs showed intermediate off-target profiles, while SpCas9 demonstrated fewer off-target counts in comparative studies [103]. Advanced Cas9 variants (e.g., High-Fidelity Cas9) and optimized gRNA designs further minimize off-target editing.
Therapeutic Validation: All three platforms have demonstrated clinical efficacy. ZFNs and TALENs have proven successful in ex vivo applications, such as generating engineered T-cells [101]. CRISPR has achieved landmark approvals with Casgevy (exa-cel) for sickle cell disease and beta-thalassemia, and shows promising results in ongoing in vivo trials for hereditary transthyretin amyloidosis (hATTR) and hereditary angioedema (HAE) [8].
Table 2: Quantitative Performance Comparison in Therapeutic Applications
| Performance Metric | ZFNs | TALENs | CRISPR-Cas9 |
|---|---|---|---|
| Design Complexity | High (complex protein engineering) | Moderate (modular protein assembly) | Low (simple gRNA design) |
| Development Timeline | ~1 month or more [54] | ~1 month [54] | Within a week [54] |
| Relative Cost | High [102] [54] | Medium [54] | Low [102] [54] |
| Multiplexing Capacity | Limited | Limited | High (multiple gRNAs) |
| Typical Editing Efficiency | Variable | High in optimized designs | Generally high across targets |
| Off-Target Profile | Lower than CRISPR [54] | Lower than CRISPR [54] | Higher, but improvable with engineered variants [54] |
| Delivery Constraints | Moderate (smaller than TALENs) | Challenging (large size) | Moderate (Cas9 + gRNA) |
| Clinical Validation | Yes (ex vivo therapies) | Yes (ex vivo therapies) | Yes (ex vivo and in vivo therapies) |
Experimental Protocols
Protocol 1: Design and Assembly of Editing Constructs
ZFN Assembly Protocol
- Step 1: Identify target sequence using ZFN design tools (e.g., ZiFiT). Target sites consist of two inverted ZFN binding sites separated by a 5-6 bp spacer [101].
- Step 2: Select zinc finger modules from validated libraries recognizing 5'-GNN-3' triplets. Assembly typically involves 3-6 fingers per ZFN monomer to achieve 9-18 bp recognition [101] [54].
- Step 3: Clone zinc finger arrays into expression vectors containing FokI nuclease domain. Utilize obligate heterodimer FokI variants (e.g., ELD:KKR) to minimize off-target cleavage [101].
- Step 4: Validate DNA binding affinity via electrophoretic mobility shift assay (EMSA) and nuclease activity using reporter cell lines.
TALEN Assembly Protocol
- Step 1: Identify target sequence beginning with 5'-T followed by 13-20 bp recognized by each TALEN monomer, separated by a 12-19 bp spacer [101].
- Step 2: Assemble TALE repeat arrays using modular cloning systems (Golden Gate assembly). Assign RVDs based on target nucleotide: NI for A, HD for C, NG for T, NN for G [101] [54].
- Step 3: Clone TALE arrays into vectors containing FokI nuclease domain. Incorporate +136 C-terminal truncation to enhance activity while maintaining specificity [101].
- Step 4: Validate constructs via SURVEYOR or T7E1 mismatch cleavage assays in mammalian cells.
CRISPR-Cas9 gRNA Design and Vector Construction
- Step 1: Identify 20-nt target sequences adjacent to 5'-NGG-3' PAM using design tools (e.g., CRISPOR). Prioritize targets with minimal off-target potential.
- Step 2: Synthesize gRNA oligonucleotides and clone into Cas9 expression vectors (e.g., pX330, pSpCas9(BB)).
- Step 3: For therapeutic applications, consider high-fidelity Cas9 variants (e.g., SpCas9-HF1, eSpCas9) to minimize off-target effects [45].
- Step 4: Validate gRNA activity using T7E1 assay or tracking of indels by decomposition (TIDE) analysis.
Diagram 1: Therapeutic gene editing workflow. This flowchart illustrates the standardized process from target identification through validation, applicable to all major editing platforms.
Protocol 2: Delivery Methods for Therapeutic Applications
Efficient delivery remains a critical challenge in therapeutic gene editing. The choice of delivery method depends on the target cells, editing platform, and therapeutic approach (in vivo vs. ex vivo) [51] [45]:
Viral Vector Delivery
- Adeno-Associated Viruses (AAVs): Suitable for in vivo delivery of ZFNs and compact TALENs. Limited packaging capacity (~4.7 kb) constrains delivery of larger editors. AAVs are ideal for CRISPR systems using smaller Cas orthologs (e.g., SaCas9) [45].
- Lentiviruses (LVs): Accommodate larger inserts, enabling TALEN delivery. Provide stable integration but raise safety concerns for therapeutic use. Ideal for ex vivo applications [45].
Non-Viral Delivery
- Lipid Nanoparticles (LNPs): Emerging as the preferred method for in vivo CRISPR delivery. Recent clinical successes include Intellia's hATTR and HAE therapies, where LNPs demonstrated efficient liver-targeted delivery with potential for redosing [8] [51].
- Electroporation: Highly efficient for ex vivo delivery to hematopoietic stem cells and T-cells. Proven successful in clinical trials for Casgevy (exa-cel) [45] [32].
Table 3: Delivery Methods for Therapeutic Gene Editing Platforms
| Delivery Method | Applicable Platforms | Therapeutic Context | Advantages | Limitations |
|---|---|---|---|---|
| AAV Vectors | ZFNs, Compact TALENs, CRISPR (small Cas variants) | In vivo | High transduction efficiency, tissue-specific targeting | Limited packaging capacity, immunogenicity concerns |
| Lentiviral Vectors | TALENs, ZFNs, CRISPR | Ex vivo, some in vivo | Large packaging capacity, stable expression | Insertional mutagenesis risk, immunogenicity |
| Lipid Nanoparticles (LNPs) | CRISPR, mRNA-encoded editors | In vivo | Low immunogenicity, redosing potential, clinical validation | Primarily liver-tropic without modification |
| Electroporation | All platforms (as DNA, RNA, or RNP) | Ex vivo | High efficiency, direct delivery, controlled exposure | Cell type-dependent toxicity, not suitable for in vivo |
The Scientist's Toolkit: Research Reagent Solutions
Successful implementation of gene editing technologies requires carefully selected reagents and tools. The following table outlines essential solutions for therapeutic editing applications:
Table 4: Essential Research Reagents for Gene Editing Applications
| Reagent Category | Specific Examples | Function | Therapeutic Application Notes |
|---|---|---|---|
| Nuclease Expression Systems | pZFN and pTALEN plasmids; pX330 (Cas9+gRNA) | Engineered nuclease delivery | GMP-grade plasmids available for clinical applications [104] |
| Delivery Reagents | AAV serotypes (AAV2, AAV8, AAV9); LNPs (IONizable lipids); Electroporation systems (Neon, Amaxa) | Facilitate cellular entry of editing components | LNP-CRISPR formulations enable in vivo delivery (e.g., CTX310 for hATTR) [8] [32] |
| Validation Assays | T7E1 mismatch detection; GUIDE-seq; NGS validation panels | Assess on-target efficiency and off-target effects | GUIDE-seq adapted for ZFN/TALEN off-target profiling [103] |
| Stem Cell Culture Systems | mTeSR1; StemFlex; Recombinant vitronectin | Maintain pluripotency during editing | Critical for ex vivo therapies like Casgevy [32] |
| HDR Enhancement Reagents | Alt-R HDR Enhancer; RS-1 | Improve homology-directed repair efficiency | Increase precise editing rates for knock-in therapies |
| Cell Sorting & Isolation | FACS systems; Magnetic bead isolation (MACS) | Enrich successfully edited cells | Clinical-scale systems for therapeutic cell products |
Diagram 2: Gene editing mechanism comparison. All platforms converge on creating double-strand breaks but differ in their target recognition mechanisms, ultimately engaging shared cellular repair pathways.
The landscape of therapeutic gene editing continues to evolve rapidly, with each platform offering distinct advantages for specific applications. CRISPR-Cas9 currently dominates therapeutic development due to its simplicity, versatility, and continuous innovation, as evidenced by the growing pipeline of clinical trials targeting both rare genetic disorders and common diseases [8] [32]. However, ZFNs and TALENs maintain relevance in applications requiring validated high-specificity edits and established regulatory pathways [102] [103].
Future directions include the development of next-generation editing technologies such as base editing and prime editing, which enable precise nucleotide changes without inducing DSBs [89]. Additionally, advances in delivery systems, particularly tissue-specific LNPs and novel viral vectors, will expand the therapeutic potential of all editing platforms. As the field progresses, the optimal choice of editing platform will increasingly depend on the specific therapeutic context, target tissue, and desired genetic outcome, with all three technologies occupying complementary roles in the gene editing toolkit.
The translation of CRISPR-Cas genome editing from research tool to clinical therapeutic represents a paradigm shift in therapeutic cell design. For researchers and drug development professionals, establishing robust benchmarks for efficiency and specificity is paramount to ensuring both the safety and efficacy of these interventions. While CRISPR systems offer unprecedented precision in genetic manipulation, their clinical application hinges on comprehensive quantification of on-target editing efficiency and rigorous monitoring of off-target effects. The inherent trade-offs between these two metrics must be carefully balanced through standardized measurement methodologies and benchmark values that meet regulatory standards. This document outlines established protocols, quantitative benchmarks, and experimental frameworks for evaluating CRISPR-Cas systems within the context of developing clinically viable therapeutic cell products.
Quantitative Benchmarks for CRISPR-Cas Performance
The performance of CRISPR-Cas systems in clinical development is quantified through two primary metrics: on-target editing efficiency (the percentage of intended genetic modifications at the target locus) and specificity (the absence of unintended modifications at off-target sites). Establishing benchmarks for these parameters requires standardized measurement approaches.
Table 1: Established Benchmark Ranges for CRISPR-Cas Systems in Clinical Development
| Parameter | Target Benchmark | Measurement Technology | Clinical Context |
|---|---|---|---|
| On-Target Efficiency | >70% modification of alleles [8] | Next-Generation Sequencing (NGS) of target locus | Ex vivo editing of hematopoietic stem cells for sickle cell disease [8] |
| Off-Target Specificity | No detectable off-target activity above background [37] | Genome-wide assays (e.g., GUIDE-seq, CIRCLE-seq) [105] | Preclinical safety assessment for in vivo therapies [37] |
| Protein Reduction (In Vivo) | ~90% reduction in disease-related protein [8] | Immunoassays (e.g., ELISA) on blood serum | Systemic LNP delivery for hATTR amyloidosis [8] |
| Translational Burden | Minimize DNA/RNA bulges in off-target sites [105] | Specialized NGS analysis | Improving sgRNA design and specificity prediction |
For on-target efficiency, deep amplicon sequencing of the target genomic region remains the gold standard. In successful clinical applications, such as the ex vivo treatment for sickle cell disease, high modification rates of the target allele are critical for therapeutic benefit [8]. For specificity, the benchmark is the absence of off-target indels above the method's detection limit, which for sensitive assays like CIRCLE-seq can be as low as 0.0017% of reads [105]. It is critical to note that optimal benchmarks can be context-dependent, varying with the specific Cas nuclease, delivery method, and target cell type.
Experimental Protocols for Assessing Efficiency and Specificity
Protocol: Measuring On-Target Editing Efficiency via NGS
This protocol details the steps for quantifying the efficiency of CRISPR-induced indels at a specific genomic locus.
Sample Preparation (Day 1-3):
- Cell Harvesting: After CRISPR delivery and a suitable incubation period (e.g., 72 hours), harvest the edited cells and extract genomic DNA using a commercial kit. Quantify DNA concentration using a fluorometer.
- PCR Amplification: Design primers flanking the CRISPR target site to generate an amplicon of 300-500 bp. Perform a primary PCR to amplify the region of interest from the purified genomic DNA.
Library Preparation & Sequencing (Day 4-6):
- Indexing PCR: Attach unique dual indices (UDIs) and sequencing adapters to the amplicons in a second, limited-cycle PCR reaction. This allows for multiplexing of samples.
- Library Purification & QC: Clean up the final library using solid-phase reversible immobilization (SPRI) beads. Quantify the library using qPCR and check its size distribution using a bioanalyzer or fragment analyzer.
- Sequencing: Pool libraries at equimolar concentrations and sequence on an Illumina MiSeq or HiSeq platform to achieve high coverage (>50,000x read depth per sample).
Data Analysis (Day 7):
- Demultiplexing: Assign reads to samples based on their unique indices.
- Alignment & Quantification: Use a specialized tool (e.g., CRISPResso2, amplicon indel analyzer) to align sequencing reads to the reference sequence and quantify the percentage of reads containing insertions, deletions, or other modifications precisely at the cut site. The editing efficiency is calculated as: (Number of reads with indels / Total aligned reads) × 100.
Protocol: Genome-Wide Off-Target Cleavage Detection using GUIDE-seq
GUIDE-seq (Genome-wide, Unbiased Identification of DSBs Enabled by sequencing) is a highly sensitive, cell-based method for detecting off-target sites [105].
Transfection & Integration (Day 1-2):
- Co-transfect cultured cells with the following complexes:
- Cas9 ribonucleoprotein (RNP) complex (Cas9 protein + sgRNA).
- A blunt-ended, double-stranded oligodeoxynucleotide (dsODN) tag.
- The dsODN tag is preferentially integrated into double-strand breaks (DSBs) generated by Cas9 during the cell's repair process. Incubate cells for 48 hours.
- Co-transfect cultured cells with the following complexes:
Genomic DNA Extraction & Shearing (Day 3):
- Harvest transfected cells and extract high-molecular-weight genomic DNA.
- Fragment the DNA by sonication to an average size of 500 bp.
Library Preparation & Enrichment (Day 4-5):
- Library Construction: Prepare a standard Illumina sequencing library from the sheared DNA: end-repair, A-tailing, and adapter ligation.
- Enrichment for Tag-Integrated Sites: Perform two nested PCRs using primers specific to the integrated dsODN tag and the Illumina adapter to selectively amplify genomic regions that have captured the tag.
- Purification and QC: Purify the final PCR product and validate its quality.
Sequencing & Analysis (Day 6-8):
- Sequence the enriched library on a high-throughput sequencer.
- Bioinformatic Analysis: Process the sequencing data using the published GUIDE-seq computational pipeline. The pipeline maps the sequenced reads to the reference genome, identifies genomic locations flanked by the dsODN tag sequence, and reports all off-target sites. These sites should be validated by targeted amplicon sequencing.
The following workflow diagram illustrates the key experimental steps in the GUIDE-seq protocol:
The Scientist's Toolkit: Essential Research Reagents
Successful execution of CRISPR assays requires a suite of well-characterized reagents. The table below lists key materials and their functions for critical experiments.
Table 2: Essential Research Reagents for CRISPR-Cas Assays
| Reagent / Solution | Function | Application Example |
|---|---|---|
| Cas9 Nuclease (RNP) | The active editing complex; using pre-formed RNP improves kinetics and can reduce off-target effects. | Direct delivery into primary cells (e.g., T cells, HSCs) for ex vivo editing. |
| dsODN Tag (e.g., GUIDE-seq) | A blunt, double-stranded oligodeoxynucleotide that integrates into Cas9-induced DSBs, marking them for sequencing-based identification. | Genome-wide off-target detection using the GUIDE-seq protocol [105]. |
| Lipid Nanoparticles (LNPs) | A non-viral delivery vector for in vivo administration of CRISPR components (mRNA/sgRNA or RNP). | Systemic delivery for liver-targeted therapies, such as hATTR amyloidosis treatment [8]. |
| High-Fidelity DNA Polymerase | For accurate and unbiased amplification of target loci during NGS library preparation. | Generating amplicons for deep sequencing to quantify on-target and validated off-target edits. |
| Validated Positive Control gRNA | A gRNA with a well-characterized on-target and off-target profile, used for assay calibration and system validation. | Benchmarking the performance and sensitivity of a new experimental setup. |
| Anti-CRISPR Proteins | Proteins that inhibit Cas nuclease activity; used as reversible controls or to limit editing windows. | Controlling the duration of Cas9 activity to enhance specificity in research models [7]. |
Navigating the Specificity Landscape: Classification and Detection
Understanding the diversity of CRISPR systems is crucial for selecting the right nuclease for a clinical application. Systems are broadly classified into Class 1 (multi-subunit effector complexes, e.g., Type I, III, IV) and Class 2 (single-protein effectors, e.g., Type II Cas9, Type V Cas12, Type VI Cas13) [25]. Most therapeutic applications currently utilize Class 2 systems due to their simpler delivery requirements.
The following diagram illustrates the evolutionary classification of major CRISPR-Cas types and their key characteristics relevant to specificity and application:
A critical advancement in managing specificity is the development of in silico off-target prediction tools. These tools can be categorized as alignment-based, hypothesis-driven, learning-based, or energy-based [105]. For a comprehensive analysis, an integrated platform like iGWOS (integrated Genome-Wide Off-target cleavage Search) leverages multiple algorithms to improve prediction accuracy, providing a crucial first-pass assessment of gRNA safety before costly experimental validation [105]. This computational pre-screening is now a standard step in therapeutic gRNA design.
The integration of Artificial Intelligence (AI), particularly deep learning, has revolutionized the design of guide RNAs (gRNAs) for CRISPR-Cas genome editing. This transformation is critical for advancing therapeutic cell design, where the precision and efficiency of gene editing are paramount. Traditional gRNA design methods, often reliant on simple rules and limited datasets, struggle to predict on-target efficiency and off-target effects accurately across diverse cellular contexts. AI models overcome these limitations by learning from vast, high-throughput experimental data, capturing complex sequence determinants and contextual genomic features that govern CRISPR activity [106] [107]. This capability is especially valuable for developing cell therapies, where optimized gRNAs can mean the difference between a successful therapeutic outcome and unintended genetic consequences.
Recent advances demonstrate AI's growing role. For instance, CRISPR-GPT, a large language model developed at Stanford Medicine, acts as a gene-editing "copilot," assisting researchers in generating optimized gRNA designs, analyzing data, and troubleshooting experimental flaws. This tool can flatten the steep learning curve associated with CRISPR, making high-quality gene editing more accessible even to non-experts [108]. Furthermore, AI is now being applied not only to standard Cas9 nucleases but also to more sophisticated precision editing tools like base editors and prime editors, enhancing their applicability in therapeutic development [106].
Computational Prediction of gRNA Efficacy
Deep Learning Models for On-Target Activity
Predicting gRNA on-target activity is a complex problem that depends on multiple factors, including the gRNA sequence itself, the genomic context of the target site, and the specific CRISPR system employed. Deep learning models have become the state-of-the-art solution, capable of integrating these multi-modal data sources for superior prediction accuracy.
CRISPRon is a prominent deep learning framework that exemplifies this approach. It integrates gRNA sequence features with epigenomic information, such as local chromatin accessibility, to predict Cas9 on-target knockout efficiency. By combining sequence and cellular context, the model achieves more accurate efficiency rankings of candidate guides compared to prior sequence-only predictors [107]. Another model, DeepSpCas9, utilizes a convolutional neural network (CNN) architecture trained on a massive dataset of 12,832 target sequences. This model demonstrated better generalization across different datasets compared to existing models, highlighting the value of large, high-quality training data [106].
For CRISPR base editors, which enable precise single nucleotide changes without double-strand breaks, new deep learning models have been developed to address their unique design challenges. The CRISPRon-ABE and CRISPRon-CBE models are trained to predict both gRNA editing efficiency and the frequency of specific editing outcomes for adenine base editors (ABEs) and cytosine base editors (CBEs), respectively [109] [110]. A key innovation in these models is their "dataset-aware" training, which involves simultaneous training on multiple experimental datasets while tracking the origin of each data point. This approach accounts for systematic variations between datasets resulting from different base editor variants, experimental platforms, or cell types, leading to more robust and generalizable predictions [109]. These models can predict the full spectrum of potential editing outcomes within the editing window, which is crucial for avoiding unintended "bystander" edits [110].
Table 1: Key AI Models for gRNA and Editor Design
| Model Name | Primary Application | Key Features | Key Performance Metrics |
|---|---|---|---|
| CRISPR-GPT [108] | gRNA design & experimental planning | AI copilot; beginner/expert modes; leverages 11 years of published data | Enabled successful first-attempt experiment by a novice researcher [108] |
| CRISPRon [107] | On-target efficiency (Cas9) | Integrates sequence & epigenomic features (e.g., chromatin accessibility) | More accurate efficiency ranking than sequence-only predictors [107] |
| CRISPRon-ABE/CBE [109] [110] | Base editing outcome prediction | "Dataset-aware" training on multiple datasets; predicts efficiency & outcome frequency | Superior performance on independent test sets vs. DeepABE/CBE, BE-HIVE [110] |
| OpenCRISPR-1 [9] | Novel AI-generated editor | Cas9-like effector designed with a large language model (ProGen2) | Comparable or improved activity and specificity relative to SpCas9, while being 400 mutations away in sequence [9] |
| DeepXE [111] | Editing efficiency for CasXE editors | AI-driven platform for engineered CasXE editors | >90% sensitivity, halved screening size, doubled hit rates, <10% false negatives [111] |
Protocol: Implementing a gRNA Design Workflow with AI
This protocol outlines a standard workflow for designing high-efficacy gRNAs for a therapeutic gene knockout in human T cells using a combination of publicly available AI tools.
Step 1: Target Site Identification
- Input the genomic sequence of the target gene (e.g., PDCD1 for PD-1 knockout in CAR-T cells) into a gRNA design tool such as the CRISPRon web server [107].
- Define design constraints, including the specific Cas nuclease (e.g., SpCas9) and the need to avoid SNPs or repetitive regions.
Step 2: In silico gRNA Screening and Prioritization
- The AI tool will output a list of candidate gRNAs with predicted on-target efficiency scores.
- Use integrated off-target prediction algorithms (e.g., Cutting Frequency Determination - CFD score) to assess each candidate gRNA for potential off-target sites across the reference genome [106].
- Prioritize gRNAs that balance high predicted on-target activity with minimal off-target sites and a high specificity score.
Step 3: Specificity and Context Validation
- For advanced therapeutic applications, incorporate additional genomic context features. If the model supports it, input cell-type-specific epigenetic data (e.g., chromatin accessibility from ATAC-seq data of primary T cells) to refine predictions [107].
- Cross-reference the top gRNA designs with databases of known genetic variants to avoid targeting sequences with common polymorphisms.
Step 4: Experimental Validation
- Synthesize the top 3-5 ranked gRNAs.
- Electroporate the gRNAs as ribonucleoprotein (RNP) complexes with Cas9 protein into primary human T cells.
- After 72 hours, extract genomic DNA and assess editing efficiency at the on-target site using T7 Endonuclease I assay or next-generation sequencing (NGS).
- Perform NGS-based off-target analysis on the top predicted potential off-target sites to empirically confirm specificity.
AI in Designing Novel CRISPR Systems
Beyond optimizing gRNAs for existing Cas enzymes, AI is now pioneering the design of novel CRISPR systems themselves. This involves using protein language models to generate entirely new Cas effectors with desirable properties for therapeutic applications.
A landmark study detailed in Nature curated a massive dataset of over 1 million CRISPR operons, termed the "CRISPR–Cas Atlas," to train a large language model (ProGen2) [9]. This model was then used to generate millions of novel CRISPR-Cas protein sequences, resulting in a 4.8-fold expansion of diversity compared to known natural proteins. From these AI-generated proteins, researchers successfully identified a functional gene editor, termed OpenCRISPR-1, which is highly functional in human cells despite being ~400 mutations away from any known natural Cas9 [9]. This demonstrates AI's power to bypass evolutionary constraints and create optimized editors from scratch.
The application of explainable AI (XAI) techniques is also enhancing the design process. XAI helps interpret the "black box" nature of deep learning models, revealing which nucleotide positions or sequence features most significantly influence gRNA activity or specificity [107]. These insights can guide the rational engineering of both gRNAs and Cas proteins, leading to safer and more effective editors for cell therapy.
Table 2: Essential Research Reagent Solutions for AI-Guided CRISPR Workflows
| Reagent / Tool Category | Example Products / Systems | Function in Workflow |
|---|---|---|
| AI Design Platforms | CRISPR-GPT [108], CRISPRon Web Server [109] [110], DeepXE [111] | Predicts gRNA efficiency/outcomes; designs novel editors; plans experiments. |
| Base Editing Systems | ABE7.10, ABE8e, BE4-Gam [109] [110] | Enables precise A•T to G•C or C•G to T•A conversion without double-strand breaks. |
| Novel AI-Generated Editors | OpenCRISPR-1 [9] | Provides highly functional, specific Cas9-like effectors designed de novo by AI. |
| Delivery Tools | Ribonucleoprotein (RNP) complexes [111], AAV vectors | Enables efficient, transient delivery of CRISPR components into primary cells like T cells. |
| Validation & Sequencing | Next-Generation Sequencing (NGS), T7E1 Assay, SURRO-seq [110] | Measures on-target and off-target editing efficiency and outcomes. |
Experimental Protocol for Validating AI-Designed gRNAs in Base Editing
This protocol details the steps for empirically testing the efficiency and product distribution of gRNAs predicted by the CRISPRon-ABE model for adenine base editing in a human cell line.
Step 1: gRNA Selection and Plasmid Construction
- Select 3-5 gRNA target sequences for a gene of interest from the CRISPRon-ABE model output, ensuring they cover a range of predicted efficiencies (e.g., high, medium, low) [110].
- Clone each gRNA sequence into a lentiviral expression plasmid containing the ABE8e editor (e.g., pCMV_ABE8e). Include a non-targeting control gRNA.
Step 2: Cell Culture and Transfection
- Culture HEK293T cells in Dulbecco's Modified Eagle Medium (DMEM) supplemented with 10% FBS at 37°C and 5% CO₂.
- Seed 2.0 x 10^5 cells per well in a 12-well plate 24 hours before transfection.
- Transfect cells with 1 µg of the ABE8e editor plasmid and 0.5 µg of the gRNA expression plasmid using a standard polyethylenimine (PEI) protocol.
Step 3: Harvest and DNA Extraction
- 72 hours post-transfection, harvest cells by trypsinization and wash with PBS.
- Extract genomic DNA using a commercial kit, eluting in 50 µL of nuclease-free water. Quantify DNA concentration.
Step 4: Amplicon Sequencing and Analysis
- Design PCR primers to amplify a ~300 bp region surrounding the gRNA target site.
- Perform PCR amplification using barcoded primers suitable for NGS. Purify the amplicons and pool equimolar amounts.
- Sequence the pooled library on an Illumina MiSeq system to achieve >2000x coverage per gRNA.
- Analyze the sequencing data using a base editing analysis pipeline (e.g., BEAT) to calculate the A-to-G editing efficiency at each target position and the frequency of all possible editing outcomes within the editing window, including bystander edits [110].
- Correlate the experimentally measured efficiencies with the AI model's predictions to validate the tool's accuracy.
The integration of AI and machine learning into gRNA design and outcome prediction marks a transformative leap forward for CRISPR-based therapeutic cell design. The emergence of sophisticated tools like CRISPR-GPT for experimental planning [108], CRISPRon for base editing prediction [109] [110], and the de novo design of novel editors like OpenCRISPR-1 [9] collectively empower researchers to achieve unprecedented levels of precision and efficiency. As these AI models continue to evolve, incorporating ever-larger datasets and more sophisticated architectures, they will undoubtedly accelerate the development of safer and more effective gene therapies, paving the way for a new era in precision medicine.
The therapeutic application of CRISPR-Cas genome editing requires rigorous safety profiling to detect unintended off-target modifications. While off-target effects have been characterized in immortalized cell lines, primary human cells present unique challenges and opportunities for safety assessment due to their normal repair processes and the clinical relevance of edited hematopoietic stem and progenitor cells (HSPCs) and T-cells for regenerative medicine and immunotherapy [112] [113]. This application note provides a comprehensive framework for off-target analysis in primary cells, detailing experimental workflows, quantitative assessment methods, and standardized protocols to ensure patient safety in clinical development.
Understanding Off-Target Effects in Primary Cell Models
Types of Unintended Editing Outcomes
CRISPR-Cas9 editing in primary cells can generate several classes of unintended effects:
- Off-target indels: Small insertions or deletions at genomic sites with sequence similarity to the intended target, resulting from Cas9 tolerating small DNA mismatches [112].
- Structural variants (SVs): Larger genomic aberrations (>50 bp) including deletions, duplications, inversions, translocations, and complex events such as chromothripsis [112]. These arise from improper repair of double-strand breaks (DSBs) either at on- or off-target sites.
- On-target complex rearrangements: Mega-base-scale deletions, insertions, chromosomal truncations, and copy-neutral loss of heterozygosity resulting from single DSBs [112].
In primary HSPCs, the frequency of kilobase-sized deletions and inversions ranges between 0.05-3%, while chromosomal truncations occur at 2-25.5% in edited clones, independent of the target locus [112]. Intra-chromosomal translocations can comprise up to 6.2-14% of editing outcomes [112].
Primary Cell Specific Considerations
Primary cells exhibit different editing outcomes compared to immortalized lines. Studies in HSPCs demonstrate that transient RNP delivery of high-fidelity Cas9, coupled with ex vivo culture up to 10 days, does not introduce or enrich for tumorigenic variants at a detectable frequency [113]. The p53 response in primary cells with functional DNA damage sensing differs from immortalized lines, which may have pre-existing mutations that provide selective advantage during editing [113].
Table 1: Comparison of Editing Outcomes in Primary vs. Immortalized Cells
| Editing Outcome | Primary HSPCs | Immortalized Lines (e.g., HEK293T) |
|---|---|---|
| On-target efficiency | High (e.g., 40-90% indels with RNP) [113] | Variable, often high |
| Kilobase deletions | Not detected in ultra-deep sequencing [113] | ~3% frequency [112] |
| Chromosomal truncations | Not systematically assessed | 10-25.5% in clones [112] |
| Translocations | Not detected in cancer gene panels [113] | 6.2-14% of outcomes [112] |
| p53 response | Functional, may reduce viability of damaged cells [113] | Often compromised, may enrich for mutations [113] |
Experimental Design for Comprehensive Off-Target Assessment
Cell Source and Culture Conditions
- HSPC sources: CD34+-purified umbilical cord blood, mobilized peripheral blood, or bone marrow [113]
- T-cell sources: Peripheral blood mononuclear cells (PBMCs) isolated from whole blood, buffy coat, or leukapheresis samples [114]
- Culture media: Use specialized expansion media (e.g., ImmunoCult-XF T Cell Expansion Medium for T-cells [114])
- Activation requirements: T-cells require activation (e.g., CD3/CD28 stimulation) for efficient editing [114]
- Timepoints: Harvest genomic DNA at days 4 and 10 post-editing to assess variant enrichment during ex vivo expansion [113]
CRISPR Delivery Optimization
Ribonucleoprotein (RNP) complex electroporation is the preferred method for primary cells:
- Advantages: Transient activity, reduced off-target effects, high efficiency, minimal toxicity [113] [114]
- Components: Recombinant high-fidelity Cas9 protein complexed with synthetic guide RNA [113] [114]
- gRNA format: Synthetic sgRNA or crRNA:tracrRNA duplexes avoid 5' triphosphate-mediated immune activation [114]
Experimental Workflow
The following diagram illustrates the complete experimental workflow for off-target assessment in primary cells:
Methods for Off-Target Detection and Quantification
Sequencing-Based Detection Methods
Multiple complementary approaches are required for comprehensive off-target profiling:
Table 2: Off-Target Detection Method Comparison
| Method | Principle | Detection Capability | Depth/Sensitivity | Primary Cell Compatibility |
|---|---|---|---|---|
| TSO500 targeted sequencing [113] | Hybrid-capture of 523 cancer-associated genes | SNVs, indels, MNVs, amplifications | <0.1% VAF | Excellent - adapted for primary cell gDNA |
| Whole exome sequencing (WES) [113] | Sequencing all exonic regions | Coding region variants | ~1% VAF | Good |
| Whole genome sequencing (WGS) [113] | Genome-wide sequencing | All variant types including intergenic | ~1% VAF | Good, but expensive |
| GUIDE-seq [115] | Capturing off-target breaks by oligonucleotide integration | Genome-wide off-target sites | High sensitivity | Limited - requires efficient tag integration |
| CIRCLE-seq [115] | In vitro identification using circularized DNA | Cell-free off-target site prediction | Highly sensitive | Indirect assessment only |
Quantitative Assessment of Editing Safety
Data from HSPC editing studies demonstrate the safety of optimized approaches:
Table 3: Quantitative Safety Assessment in Primary HSPCs
| Assessment Parameter | AAVS1 Targeting | HBB Targeting | ZFPM2 Targeting | Control (Mock) |
|---|---|---|---|---|
| On-target indel efficiency [113] | High (40-90%) | High (40-90%) | Lower efficiency | 0% |
| On-target SNV frequency [113] | Not significantly different from control | Not significantly different from control | Not significantly different from control | Baseline |
| On-target MNV frequency [113] | Not significantly different from control | Not significantly different from control | Not significantly different from control | Baseline |
| Indels in 523 cancer genes [113] | Not detected above control | Not detected above control | Not detected above control | Baseline |
| EZH2 exon 5 variants (predicted ZFPM2 off-target) [113] | Not applicable | Not applicable | Not detected | Not applicable |
Step-by-Step Protocol: Off-Target Analysis in Primary T-Cells and HSPCs
Primary T-Cell Isolation and Activation (Duration: 3 days)
Materials:
- EasySep Human T Cell Isolation Kit [114]
- ImmunoCult-XF T Cell Expansion Medium [114]
- ImmunoCult Human CD3/CD28 T Cell Activator [114]
- Human Recombinant IL-2 [114]
Procedure:
- Isolate human T-cells from peripheral blood using immunomagnetic selection per manufacturer's instructions [114].
- Count cells and adjust to 1 × 10^6 cells/mL in pre-warmed ImmunoCult-XF T Cell Expansion Medium supplemented with 2mM L-glutamine, 50μg/mL gentamicin, and 10 ng/mL Human Recombinant IL-2 [114].
- Activate T-cells by adding 25 μL/mL of ImmunoCult Human CD3/CD28 T Cell Activator [114].
- Incubate cell suspension at 37°C and 5% CO2 for 72 hours [114].
- Optional: Assess T-cell activation by flow cytometry using anti-CD25 antibody [114].
RNP Complex Preparation and Electroporation (Duration: 1 day)
Materials:
- Synthetic sgRNA or crRNA:tracrRNA (200 μM stock) [114]
- High-fidelity Cas9 protein [113] [114]
- Electroporation system (Neon Transfection System or 4D-Nucleofector) [114]
Procedure:
- Resuspend synthetic gRNA in nuclease-free water to 100 μM (sgRNA) or 200 μM (crRNA:tracrRNA) [114].
- For crRNA:tracrRNA systems: Combine 1 μL of 200 μM crRNA with 1 μL of 200 μM tracrRNA and 3 μL annealing buffer. Heat to 95°C for 5 minutes, then cool slowly to room temperature [114].
- Prepare RNP complex by combining:
- 3 μL of 100 μM sgRNA OR 2 μL annealed crRNA:tracrRNA
- 2 μL of 10 μg/μL Cas9 protein
- 5 μL resuspension buffer [114]
- Incubate at room temperature for 10-20 minutes to form RNP complexes.
- Electroporate 1-2 × 10^5 cells using manufacturer-optimized settings for primary T-cells or HSPCs [114].
- Immediately transfer cells to pre-warmed culture medium and incubate at 37°C [114].
Genomic DNA Harvest and Quality Control
Timepoints: Day 4 (indel saturation) and Day 10 (enrichment assessment) post-electroporation [113] Cell input: 3-4 × 10^5 cells per condition for ultra-deep sequencing [113] DNA quantification: Use fluorometric methods to ensure accurate concentration measurement Quality assessment: Confirm A260/A280 ratio of 1.8-2.0 and A260/A230 ratio of 2.0-2.2
Sequencing Library Preparation and Data Analysis
TSO500 Library Preparation [113]:
- Input 10-30 ng gDNA into TruSight Oncology 500 library prep
- Perform hybrid capture with 523-gene panel
- Sequence to high depth (>1000× coverage) using paired-end sequencing
Bioinformatic Analysis:
- Align sequences to reference genome (hg19)
- Call variants using unique molecular indexes to eliminate PCR duplicates
- Filter variants against mock-electroporated controls
- Focus analysis on coding sequences and splice sites of cancer-associated genes
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents for Primary Cell Off-Target Analysis
| Reagent/Category | Specific Examples | Function & Application |
|---|---|---|
| Cell Isolation Kits | EasySep Human T Cell Isolation Kit [114] | Immunomagnetic selection of primary T-cells from PBMCs |
| Cell Culture Media | ImmunoCult-XF T Cell Expansion Medium [114] | Specialized formulation for primary T-cell growth and expansion |
| Cell Activation | ImmunoCult CD3/CD28 T Cell Activator [114] | Polyclonal T-cell activation required for efficient genome editing |
| CRISPR Components | ArciTect sgRNA/crRNA [114], High-fidelity Cas9 [113] | Synthetic guide RNAs and nuclease for RNP complex formation |
| Electroporation Systems | Neon Transfection System [114], 4D-Nucleofector [114] | Delivery of RNP complexes into primary cells |
| Sequencing Kits | TruSight Oncology 500 [113] | Targeted sequencing of 523 cancer-associated genes |
| Analysis Software | COSMID [113], Cas-OFFinder [115] | In silico prediction of potential off-target sites |
Comprehensive off-target analysis in primary cells requires an integrated approach combining careful experimental design, optimized delivery methods, and multiple complementary detection technologies. The protocol outlined here provides a framework for rigorous safety assessment that can be adapted to various primary cell types and editing applications. As CRISPR-based therapies advance through clinical development, these standardized approaches to off-target profiling will be essential for ensuring patient safety and regulatory approval.
The clinical development of CRISPR-based therapies represents a frontier in modern medicine, offering the potential to treat genetic disorders at their root cause. However, the path from laboratory research to clinical trial approval is paved with rigorous regulatory requirements designed to ensure patient safety and therapeutic efficacy. The existing U.S. Food and Drug Administration (FDA) clinical development framework, originally designed for small molecule drugs, presents unique challenges when applied to complex CRISPR cell and gene therapies [30]. Regulatory guidance continues to evolve as agencies worldwide work to optimize frameworks and initiatives that can streamline the production of these innovative treatments while maintaining stringent safety standards [30].
The regulatory journey for a CRISPR therapy begins years before human trials, requiring extensive validation at each development stage. This application note details the specific validation requirements and methodologies essential for obtaining clinical trial approval, providing researchers and drug development professionals with a structured framework for navigating this complex process. Within the broader context of CRISPR-Cas genome editing in therapeutic cell design research, understanding these regulatory considerations is paramount for successfully translating laboratory breakthroughs into viable clinical treatments.
Preclinical Validation Requirements
Before a CRISPR-based therapy can be administered to human subjects, researchers must complete extensive preclinical validation to demonstrate both safety and biological activity. This stage involves multiple layers of testing and documentation to satisfy regulatory requirements for an Investigational New Drug (IND) application.
Analytical Method Validation for CRISPR Editing Assessment
Validating the precision and efficiency of genome editing is a cornerstone of preclinical development. Multiple analytical methods are employed to characterize editing outcomes, each with distinct advantages and applications. The selection of appropriate validation methods depends on the specific editing approach (NHEJ, HDR, or base editing) and the level of resolution required.
Table 1: CRISPR Analysis Methods for Editing Validation
| Method | Principle | Applications | Regulatory Considerations |
|---|---|---|---|
| Next-Generation Sequencing (NGS) | High-throughput deep sequencing of target regions | Comprehensive identification of on-target edits and off-target effects; gold standard for characterization [96] | Provides definitive evidence of editing precision; required for IND-enabling studies |
| Inference of CRISPR Edits (ICE) | Computational analysis of Sanger sequencing trace files [96] | Quantification of indel frequency and distribution; suitable for knockout validation [96] | ICE scores highly correlate with NGS (R² = 0.96) [96]; cost-effective for early screening |
| T7 Endonuclease 1 (T7E1) Assay | Enzyme-based cleavage of mismatched DNA heteroduplexes [96] [116] | Rapid, low-cost assessment of editing presence; initial screening during optimization [96] | Considered non-quantitative; insufficient as standalone evidence for clinical trials [96] |
| Restriction Fragment Length Polymorphism | Loss or gain of restriction enzyme sites through editing [117] | Detection of specific point mutations or small insertions [117] | Requires specific sequence context; often used with silent "passenger" edits to create screening markers [117] |
The following workflow outlines the strategic approach to CRISPR editing validation from initial screening to comprehensive analysis:
In Vitro and In Vivo Efficacy and Safety Studies
Beyond analytical validation of the editing process itself, CRISPR therapies must demonstrate therapeutic potential in biologically relevant systems. The FDA requires proof-of-concept studies in models that accurately recapitulate the disease biology.
For in vitro studies, researchers must use appropriate cell models, preferably primary cells from patients with the target disease, to demonstrate that CRISPR editing corrects the underlying molecular defect and results in functional improvement [118]. These studies should establish a preliminary dose-response relationship and define the therapeutic window.
In vivo studies in animal models must demonstrate both efficacy and preliminary safety. The selection of animal models is critical—they must accurately reflect the human disease genotype, phenotype, and progression [118]. For diseases affecting physiological systems unique to primates, testing in non-human primates may be required [118]. Key endpoints include:
- Efficacy Metrics: Reduction in disease biomarkers, improvement in clinical symptoms, survival benefit
- Safety Metrics: Absence of treatment-related adverse events, histopathological assessment of target tissues, monitoring for potential off-target effects
Notably, technical limitations such as mosaicism (incomplete editing), variable on-target efficiency, and off-target effects must be thoroughly characterized and minimized, as these factors significantly impact regulatory decision-making [119].
Regulatory Pathway and Documentation
FDA Engagement and IND Submission Process
Navigating the regulatory pathway for CRISPR therapies requires strategic engagement with the FDA throughout the development process. The journey from preclinical research to clinical trial approval involves multiple formal and informal interactions with regulatory agencies.
Table 2: FDA Meeting Types for CRISPR Therapy Development
| Meeting Type | Timing | Purpose | Key Discussion Points |
|---|---|---|---|
| INTERACT (Initial Targeted Engagement for Regulatory Advice on CBER Products) | Informal meeting during preclinical development [118] | Obtain preliminary feedback on CMC, pharmacology, toxicology, and clinical plans [118] | Proposed manufacturing process, preclinical study design, preliminary safety assessment |
| Pre-IND Meeting | Formal meeting before IND submission [118] | Determine if preclinical data package supports clinical trial initiation [118] | Adequacy of efficacy and safety data, clinical trial design, CMC controls, GMP compliance |
| IND Submission | Formal application to begin human trials [118] | Request authorization to administer investigational product to humans [118] | Comprehensive data from preclinical studies, manufacturing information, clinical protocol |
| Clinical Hold | FDA response to IND | Delay or prevention of clinical trial initiation [118] | Address deficiencies in safety data, manufacturing quality, or trial design |
The following diagram illustrates the complete regulatory pathway from discovery research to clinical trials:
Chemistry, Manufacturing, and Controls (CMC) Requirements
The manufacturing process for CRISPR therapies must adhere to stringent quality standards to ensure product consistency, purity, and potency. Current Good Manufacturing Practice (cGMP) regulations govern the production of all components, including Cas nucleases, guide RNAs, and delivery vehicles [30].
For CRISPR-based products, key CMC considerations include:
- Guide RNA Quality: GMP-grade gRNAs with extensive documentation of purity, sequence verification, and absence of contaminants are required for clinical trials [118]. The shift from Research Use Only (RUO) to GMP-grade materials represents a critical transition in the development pathway.
- Delivery System Characterization: Whether using viral vectors (AAV, lentivirus) or non-viral methods (lipid nanoparticles), the delivery system must be thoroughly characterized for efficiency, tropism, and potential immunogenicity [8].
- Potency Assays: Established quantitative methods must demonstrate that the final product produces the intended biological effect, typically through in vitro editing efficiency assessments in relevant cell lines.
- Stability Studies: Data must support the product's stability through manufacturing, storage, and administration, with defined shelf life and storage conditions.
The complexity of GMP requirements has created supply challenges for CRISPR therapy developers, with demand for true GMP reagents rapidly outstripping supply [30]. Vendor selection is critical, as changing suppliers between research and clinical stages can introduce variability that compromises product consistency and regulatory approval [30].
Analysis of Recent Clinical Cases
Safety Events and Regulatory Responses
Recent clinical trials illustrate the critical importance of comprehensive safety validation and the regulatory consequences when safety concerns emerge. These cases provide valuable lessons for researchers designing preclinical validation strategies.
In 2025, Intellia Therapeutics paused two Phase 3 trials of its CRISPR-Cas therapy for transthyretin amyloidosis (nexiguran ziclumeran) after a patient experienced severe liver toxicity characterized by elevated enzymes and bilirubin [7]. This Grade 4 adverse event triggered immediate regulatory engagement, with enrollment halted pending investigation and implementation of additional safety measures [7]. Despite this setback, the lipid nanoparticle delivery system was not immediately suspected, highlighting the complex safety profile of in vivo CRISPR therapies [7].
Conversely, Verve Therapeutics' VERVE-101, an adenine base editor designed to inactivate the PCSK9 gene for cholesterol management, faced clinical holds due to laboratory abnormalities associated with treatment [6]. The company responded by pausing enrollment and shifting focus to VERVE-102, which utilizes a different GalNAc-LNP delivery system [6]. Early results from VERVE-102 have been more promising, with no serious adverse events reported in the first two dose cohorts [6].
Successful Validation Strategies
Positive examples of CRISPR therapy validation demonstrate the pathway to successful regulatory approval:
The landmark case of a personalized in vivo CRISPR therapy for an infant with CPS1 deficiency developed by the Innovative Genomics Institute successfully navigated regulatory requirements by employing a comprehensive validation strategy [8]. The therapy received FDA approval and was delivered to the patient in just six months—an exceptionally rapid timeline achieved through meticulous preclinical characterization [8]. Key success factors included:
- Use of lipid nanoparticle (LNP) delivery allowing for multiple doses without the immune reactions associated with viral vectors [8]
- Demonstration of improved symptoms with each additional dose, indicating a controllable and titratable therapeutic effect [8]
- Multi-institutional collaboration that provided robust validation across independent laboratories [8]
Similarly, Intellia Therapeutics' phase I trial for hereditary transthyretin amyloidosis (hATTR) demonstrated sustained ~90% reduction in disease-related protein levels across all 27 participants who reached two-year follow-up, with no evidence of diminishing effect over time [8]. This compelling durability data supported the transition to Phase III trials by providing robust evidence of long-term efficacy and safety.
Essential Research Reagent Solutions
The successful development of CRISPR-based therapies depends on access to high-quality, well-characterized reagents that meet regulatory standards throughout the development pipeline.
Table 3: Essential Research Reagents for CRISPR Therapy Development
| Reagent Category | Key Functions | Regulatory Grade Considerations |
|---|---|---|
| Guide RNAs (gRNAs) | Targets Cas nuclease to specific genomic sequences; determines editing specificity [30] | RUO for discovery; GMP-grade for clinical trials with documentation of purity, sequence verification, and absence of endotoxins [118] [30] |
| Cas Nucleases | Creates double-strand breaks or targeted nucleotide modifications [30] | High-purity preparations with minimal lot-to-lot variability; engineered variants with reduced off-target activity may be preferred [117] |
| Delivery Systems | Enables cellular uptake of editing components (viral vectors, LNPs) [8] | Thorough characterization of efficiency, tropism, and immunogenicity; LNP systems enable redosing unlike viral vectors [8] |
| Cell Culture Media | Supports growth and maintenance of target cells during editing process | Serum-free, defined formulations reduce variability; xeno-free for clinical applications |
| Analytical Standards | Validates performance of quality control assays | Reference materials with documented editing outcomes for assay calibration and qualification |
The regulatory landscape for CRISPR-based therapies continues to evolve as the science advances and clinical experience accumulates. Successful navigation of validation requirements for clinical trial approval demands rigorous scientific characterization, strategic regulatory engagement, and meticulous attention to manufacturing quality. The cases discussed herein demonstrate both the challenges and opportunities in this rapidly advancing field.
Future developments will likely include more standardized approaches to off-target risk assessment, increased use of novel editing platforms such as base and prime editors, and potentially streamlined pathways for therapies addressing unmet medical needs. As regulatory agencies gain experience with CRISPR products, more specific guidance will emerge to help researchers design appropriate validation strategies. By adhering to the principles outlined in this application note—comprehensive editing characterization, biologically relevant efficacy models, and robust quality control—researchers can position their CRISPR therapies for successful regulatory approval and ultimately, patient benefit.
Conclusion
CRISPR-Cas genome editing has fundamentally transformed therapeutic cell design, demonstrated by landmark clinical successes in treating genetic disorders like sickle cell disease and beta-thalassemia. The integration of advanced delivery systems such as lipid nanoparticles and virus-like particles, coupled with high-fidelity editing enzymes and sophisticated validation frameworks, continues to enhance both safety and efficacy. Future directions will focus on expanding clinical applications to common and rare diseases, refining cell-specific editing protocols, integrating AI for enhanced precision, developing scalable manufacturing processes, and establishing clear regulatory pathways. As research addresses current limitations in delivery efficiency and off-target effects, CRISPR-based therapies are poised to advance toward broader clinical implementation, potentially offering cures for previously untreatable genetic conditions through precise genomic medicine.
References
- 1. Nobel Prize Awarded to Jennifer Doudna And Emmanuelle ... [https://www.synthego.com/blog/gene-editing-nobel-prize/]
- 2. Press release: The Nobel Prize in Chemistry 2020 [https://www.nobelprize.org/prizes/chemistry/2020/press-release/]
- 3. Who We Are [https://crisprtx.com/who-we-are]
- 4. Advancing CRISPR genome editing into gene therapy clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12094669/]
- 5. CMN Weekly (10 October 2025) [https://crisprmedicinenews.com/news/cmn-weekly-10-october-2025-your-weekly-crispr-medicine-news/]
- 6. CRISPR Clinical Trials to Follow [https://www.synthego.com/blog/crispr-clinical-trials/]
- 7. CMN Weekly (31 October 2025) [https://crisprmedicinenews.com/news/cmn-weekly-31-october-2025-your-weekly-crispr-medicine-news/]
- 8. CRISPR Clinical Trials: A 2025 Update [https://innovativegenomics.org/news/crispr-clinical-trials-2025/]
- 9. Design of highly functional genome editors by modelling ... [https://www.nature.com/articles/s41586-025-09298-z]
- 10. CRISPR/Cas9 & Targeted Genome Editing: New Era in ... [https://www.neb.com/en-us/tools-and-resources/feature-articles/crispr-cas9-and-targeted-genome-editing-a-new-era-in-molecular-biology?srsltid=AfmBOopXHsWn4ncB_FWowfia0J05583mEuK57IEXhuwplWO32_bZml5D]
- 11. Design Rules for Expanding PAM Compatibility in CRISPR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12424760/]
- 12. Revolution of Biotechnology with CRISPR [https://www.nature.com/articles/s12276-025-01452-x]
- 13. Exploring CRISPR-Cas: The transformative impact of gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12506487/]
- 14. Unlock CRISPR Gene Editing Potential: PAM sequences [https://www.idtdna.com/page/support-and-education/decoded-plus/crispr-cas-nucleases-understanding-pam-requirements-and-cas-diversification-strategies/]
- 15. GenomePAM directs PAM characterization and ... [https://www.nature.com/articles/s41551-025-01464-y]
- 16. HDR vs NHEJ: DNA Repair Pathway Comparison [https://invivobiosystems.com/crispr/hdr-vs-nhej/]
- 17. CRISPR-Cas9-mediated homology-directed repair for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11531618/]
- 18. Characterizing and controlling CRISPR repair outcomes in ... [https://www.nature.com/articles/s41467-025-66058-3]
- 19. CRISPR–Cas9-mediated genome editing and guide RNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4602062/]
- 20. HDR vs. NHEJ: CRISPR Gene Editing Techniques [https://www.zeclinics.com/blog/hdr-vs-nhej-in-crispr-gene]
- 21. Efficient high-precision homology-directed repair ... [https://www.nature.com/articles/s41592-023-01949-1]
- 22. How To Design Guide RNA for CRISPR [https://www.synthego.com/guide/how-to-use-crispr/design-grna-crispr/]
- 23. Strategies for High-Efficiency Mutation Using the CRISPR/ ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8860194/]
- 24. Press Release [https://ir.crisprtx.com/news-releases/news-release-details/crispr-therapeutics-announces-positive-phase-1-clinical-data]
- 25. An updated evolutionary classification of CRISPR–Cas ... [https://www.nature.com/articles/s41564-025-02180-8]
- 26. Class 2 CRISPR / Cas : an expanding biotechnology toolbox for and... [https://cellandbioscience.biomedcentral.com/articles/10.1186/s13578-018-0255-x]
- 27. A Review on the Mechanism and Applications of... [https://pubmed.ncbi.nlm.nih.gov/36163606/]
- 28. - Recent advances and Cas variants CRISPR genome editing [https://www.lubio.ch/blog/advances-in-crispr]
- 29. Recent advances in CRISPR-based single-nucleotide fidelity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12219407/]
- 30. CRISPR Cell and Gene Therapies: Key Challenges in ... [https://www.synthego.com/blog/crispr-cell-gene-therapy-obstacles/]
- 31. The CRISPR therapeutics landscape in 2025 [https://www.kilburnstrode.com/knowledge/european-ip/the-crispr-therapeutics-landscape-in-2025]
- 32. Press Release [https://ir.crisprtx.com/news-releases/news-release-details/crispr-therapeutics-provides-business-update-and-reports-third-6]
- 33. Overview CRISPR Clinical Trials 2025 - Learn | Innovate [https://crisprmedicinenews.com/clinical-trials/]
- 34. Press Release [https://ir.crisprtx.com/news-releases/news-release-details/crispr-therapeutics-present-late-breaking-data-american-heart]
- 35. Ex Vivo Cell-Based CRISPR/Cas9 Genome Editing for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7035593/]
- 36. Engineering the next-generation of CAR T-cells with ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-022-01559-z]
- 37. CRISPR/Cas9 therapeutics: progress and prospects [https://www.nature.com/articles/s41392-023-01309-7]
- 38. Gene Editing [https://crisprtx.com/gene-editing]
- 39. CRISPR/Cas-based CAR-T cells: production and application [https://pmc.ncbi.nlm.nih.gov/articles/PMC11140991/]
- 40. Leveraging CRISPR gene editing technology to optimize ... [https://www.nature.com/articles/s41375-024-02444-y]
- 41. Systematic discovery of CRISPR-boosted CAR T cell ... [https://www.nature.com/articles/s41586-025-09507-9]
- 42. Ex vivo prime editing of patient haematopoietic stem cells ... [https://www.nature.com/articles/s41551-023-01026-0]
- 43. An improved medium formulation for efficient ex vivo gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10025975/]
- 44. The hidden risks of CRISPR/Cas: structural variations and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12325979/]
- 45. Challenges and Opportunities in the Application of CRISPR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12503735/]
- 46. Lipid Nanoparticles vs. Viral Vectors: A Comparison for ... [https://www.helixbiotech.com/post/lipid-nanoparticles-vs-viral-vectors-a-comparison-for-gene-therapy]
- 47. Lipid-Nanoparticle-Based Delivery of CRISPR/Cas9 Genome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9176214/]
- 48. Advancing gene editing: the role of lipid nanoparticles in ... [https://www.drugtargetreview.com/article/188056/advancing-gene-editing-the-role-of-lipid-nanoparticles-in-crispr-delivery/]
- 49. Lung and liver editing by lipid nanoparticle delivery of a ... [https://www.nature.com/articles/s41587-024-02437-3]
- 50. CASGEVY® Clinical Trial and Results [https://www.casgevy.com/sickle-cell-disease/study-information]
- 51. Advancing gene editing therapeutics: Clinical trials and ... [https://www.sciencedirect.com/science/article/pii/S2162253125002203]
- 52. A Randomized Clinical Trial With Open-Label Extension [https://pmc.ncbi.nlm.nih.gov/articles/PMC11894486/]
- 53. Precise measurement of CRISPR genome editing ... [https://www.sciencedirect.com/science/article/pii/S2329050125000440]
- 54. Precision gene editing: The power of CRISPR-Cas in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590234/]
- 55. Emerging trends in prime editing for precision genome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12322275/]
- 56. Epigenome editing based treatment: Progresses and ... [https://www.sciencedirect.com/science/article/pii/S152500162500721X]
- 57. Programmable epigenome editing by transient delivery of ... [https://www.nature.com/articles/s41467-025-63167-x]
- 58. World's First Patient Treated with Personalized CRISPR ... [https://www.chop.edu/news/worlds-first-patient-treated-personalized-crispr-gene-editing-therapy-childrens-hospital]
- 59. Infant with rare, incurable disease is first to successfully ... [https://www.nih.gov/news-events/news-releases/infant-rare-incurable-disease-first-successfully-receive-personalized-gene-therapy-treatment]
- 60. CRISPR/Cas9 Delivery Systems to Enhance Gene Editing ... [https://pubmed.ncbi.nlm.nih.gov/40362657/]
- 61. CRISPR Delivery Methods: Cargo, Vehicles, and Challenges [https://www.synthego.com/blog/delivery-crispr-cas9/]
- 62. The hidden risks of CRISPR/Cas: structural variations and ... [https://www.nature.com/articles/s41467-025-62606-z]
- 63. A comprehensive review on the current status of CRISPR ... [https://www.sciencedirect.com/science/article/abs/pii/S014181302404902X]
- 64. CRISPR-Based Tools for Fighting Rare Diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9787644/]
- 65. CRISPR Gene Therapy: Applications, Limitations, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7427626/]
- 66. Delivery of CRISPR-Cas tools for in vivo genome editing ... [https://www.sciencedirect.com/science/article/pii/S016836592200027X]
- 67. CRISPR/Cas9 Delivery Systems to Enhance Gene Editing ... [https://www.mdpi.com/1422-0067/26/9/4420]
- 68. Customizable virus-like particles deliver CRISPR–Cas9 ... [https://www.nature.com/articles/s41565-024-01851-7]
- 69. Unlocking mRNA-driven CRISPR-Cas9 gene therapy via ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12594903/]
- 70. Targeted nonviral delivery of genome editors in vivo - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10945750/]
- 71. Off-target effects in CRISPR/Cas9 gene editing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10034092/]
- 72. CRISPR Off-Target Effects: Mechanisms and Solutions | Danaher Life Sciences [https://lifesciences.danaher.com/us/en/library/crispr-off-target-effects.html]
- 73. Understanding FDA Cell and Gene Therapy Guidance [https://www.synthego.com/blog/fda-cell-and-gene-therapy-guidance/]
- 74. Genome-wide CRISPR off-target prediction and optimization using RNA-DNA interaction fingerprints | Nature Communications [https://www.nature.com/articles/s41467-023-42695-4]
- 75. CRISPR Off-Target Editing: Prediction, Analysis, and More [https://www.synthego.com/blog/crispr-off-target-editing/]
- 76. Overcoming the Delivery Challenges in CRISPR/Cas9 Gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12434829/]
- 77. Challenges in delivery systems for CRISPR-based genome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8316527/]
- 78. innovations and challenges in rAAV vector-based CRISPR ... [https://www.nature.com/articles/s41434-025-00573-2]
- 79. Cas9 immunity creates challenges for CRISPR gene ... [https://www.nature.com/articles/s41467-018-05843-9]
- 80. Peeling back the layers of immunogenicity in Cas9-based ... [https://www.sciencedirect.com/science/article/pii/S1525001625005350]
- 81. Scientists engineer CRISPR enzymes that evade ... [https://www.broadinstitute.org/news/scientists-engineer-crispr-enzymes-evade-immune-system]
- 82. CRISPR-Edited Beta Cells Avoid Immune Rejection ... [https://crisprmedicinenews.com/news/crispr-edited-beta-cells-avoid-immune-rejection-without-immunosuppressants-in-human-transplantation/]
- 83. CRISPR-Cas systems: Overview, innovations and applications ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7508700/]
- 84. Revolutionizing in vivo therapy with CRISPR/Cas genome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10867117/]
- 85. Neurons repair CRISPR damage with unique timing [https://crisprmedicinenews.com/news/neurons-repair-crispr-damage-with-unique-timing/]
- 86. Comprehensive protocols for CRISPR/Cas9-based gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4988528/]
- 87. The Complete Guide to Understanding CRISPR sgRNA [https://www.synthego.com/guide/how-to-use-crispr/sgrna/]
- 88. CRISPR-Cas9 in Cardiovascular Medicine: Unlocking New ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11763404/]
- 89. Recent advances in therapeutic gene-editing technologies [https://www.sciencedirect.com/science/article/pii/S152500162500200X]
- 90. CRISPR sgRNA for Successful Gene Editing: Discovery to ... [https://www.synthego.com/blog/crispr-gmp-sgrna/]
- 91. CRISPR CGMP gRNA Manufacturing Services | IDT [https://www.idtdna.com/page/products/cgmp-crispr-manufacturing/cgmp-grna-manufacturing/]
- 92. cGMP CRISPR Clinical Solutions [https://www.synthego.com/cgmp-crispr-solutions/]
- 93. Cellular & Gene Therapy Guidances [https://www.fda.gov/vaccines-blood-biologics/biologics-guidances/cellular-gene-therapy-guidances]
- 94. Characterizing and controlling CRISPR repair outcomes in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12623481/]
- 95. Efficient in vivo labeling of endogenous proteins with ... [https://www.nature.com/articles/s41467-025-58945-6]
- 96. How to Pick the Best CRISPR Data Analysis Method for ... [https://www.synthego.com/guide/how-to-use-crispr/analysis-methods/]
- 97. Unveiling the cut-and-repair cycle of designer nucleases in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12583642/]
- 98. Comparative Analysis of Methods for Assessing On-Target ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11932317/]
- 99. Systematic Comparison of Computational Tools for Sanger ... [https://www.mdpi.com/2073-4409/13/3/261]
- 100. TIDES 2025 [https://www.genscript.com/tides-2025.html]
- 101. Expanding the genetic editing tool kit: ZFNs, TALENs, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4191047/]
- 102. Comparing Gene Editing Platforms: CRISPR vs. Traditional ... [https://blog.crownbio.com/comparing-gene-editing-platforms-crispr-vs-traditional-methods]
- 103. The comparison of ZFNs, TALENs, and SpCas9 by GUIDE- ... [https://www.sciencedirect.com/science/article/pii/S216225312100202X]
- 104. CMN Weekly (25 July 2025) - Your Weekly CRISPR ... [https://crisprmedicinenews.com/news/cmn-weekly-25-july-2025-your-weekly-crispr-medicine-news/]
- 105. Benchmarking and integrating genome-wide CRISPR off ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7672467/]
- 106. Revolutionizing CRISPR technology with artificial intelligence [https://www.nature.com/articles/s12276-025-01462-9]
- 107. Artificial Intelligence for CRISPR Guide RNA Design [https://arxiv.org/html/2508.20130v1]
- 108. AI-powered CRISPR could lead to faster gene therapies ... [https://med.stanford.edu/news/all-news/2025/09/ai-crispr-gene-therapy.html]
- 109. Breaking: Deep learning multi-dataset training improves ... [https://crisprmedicinenews.com/news/breaking-deep-learning-multi-dataset-training-improves-crispr-base-editing-predictions/]
- 110. Deep learning models simultaneously trained on multiple ... [https://www.nature.com/articles/s41467-025-65200-5]
- 111. CMN Weekly (19 September 2025) [https://crisprmedicinenews.com/news/cmn-weekly-19-september-2025-your-weekly-crispr-medicine-news/]
- 112. Unintended CRISPR-Cas9 editing outcomes [https://pmc.ncbi.nlm.nih.gov/articles/PMC10182114/]
- 113. Ultra-deep sequencing validates safety of CRISPR/Cas9 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9372057/]
- 114. Genome Editing of Human Primary T Cells Using CRISPR- ... [https://www.stemcell.com/genome-editing-of-human-primary-t-cells-using-the-arcitect-crispr-cas9-system.html]
- 115. Assessing and advancing the safety of CRISPR-Cas tools [https://www.nature.com/articles/s41467-023-35886-6]
- 116. A simple validation and screening method for CRISPR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11949363/]
- 117. CRISPR 101: Validating Your Genome Edit [https://blog.addgene.org/crispr-101-validating-your-genome-edit]
- 118. Understanding CRISPR Clinical Trials [https://www.synthego.com/blog/understanding-crispr-clinical-trials/]
- 119. CRISPR ethics: moral considerations for applications of a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6286228/]